AI Medical Scribes Explained: What They Are, How They Work, and Why They Matter

The healthcare industry is undergoing a major transformation, driven by rapid advancements in technology. Among the most impactful innovations is the emergence of AI medical scribes, digital tools designed to streamline clinical documentation and reduce the administrative burden on physicians. These systems are reshaping how medical professionals manage patient records, allowing more time to focus on care delivery.
As the demand for modern medical services grows, many clinicians face increased workloads and reduced face-to-face time with patients. In the United States, physicians spend an estimated 34 to 55 percent of their day on documentation and reviewing electronic medical records. This administrative burden often contributes to physician burnout and diminished efficiency.
AI medical scribes are proving to be a powerful solution. Unlike traditional note-taking, where physicians manually record patient interactions, AI scribes automatically capture and generate accurate documentation based on clinical conversations and data. These tools support operational efficiency, enhance accuracy, and free up clinicians to prioritize patient care.
Despite their potential, many clinics and healthcare organizations remain unaware of what AI medical scribes are and how they can benefit from them. As adoption continues to grow, understanding this technology is essential for healthcare providers seeking to modernize their practice and improve outcomes.
What Is an AI Scribe
An AI medical scribe is an advanced digital tool designed to automate clinical documentation for healthcare professionals. Using artificial intelligence technologies such as natural language processing and machine learning, these systems generate structured notes based on conversations between physicians and patients. Unlike traditional scribes who document manually, AI scribes listen to clinical interactions, interpret spoken language, and create accurate records that are ready for review and entry into the electronic health record.
AI scribes are also referred to as digital scribes, ambient AI scribes, or virtual scribes. While they do not fully replace the physician’s role in reviewing and finalizing documentation, they significantly reduce the manual effort required. Understanding how AI scribes work is essential for recognizing their potential to automate repetitive tasks, improve accuracy, and enhance the overall efficiency of clinical workflows.
One of the key benefits of AI scribes is their adaptability. These tools can be integrated into a variety of healthcare settings, including hospitals, outpatient clinics, and private practices, making them a scalable and versatile solution for modern documentation needs.
How AI Medical Scribes Work
AI medical scribes are designed to transform clinical documentation by combining voice recognition, speech-to-text technology, natural language processing, and context-aware algorithms. These digital tools filter out irrelevant information and generate organized, real-time notes that support physician workflows. Because AI scribes passively listen and document without requiring manual input, they are often referred to as ambient or virtual scribes.
To better understand how AI documentation tools function, here is a breakdown of the key stages in the process:
- Audio Capture
- The AI scribe begins by recording conversations between the physician and the patient. This is typically done through phone microphones. High-quality audio is critical to the success of the entire process, as it directly impacts transcription accuracy.
- Speech Recognition
- Once the audio is captured, advanced speech recognition technology processes the conversation. This phase involves identifying and distinguishing between speakers, such as the physician and patient, even when they speak with different accents or in varied tones. The speech is then converted into written text.
- Natural Language Processing
- After transcription, natural language processing is used to analyze and interpret the text. NLP helps the system extract clinically relevant information, recognize medical terminology, and distinguish between symptoms, conditions, and treatment plans. This step ensures the resulting documentation is medically accurate and contextually appropriate.
- Data Structuring
- The extracted information is then organized and mapped into separate sections on the patient note. In the Emergency Medicine setting this might mean HPI, ROS, PE, Evals/Re-evals, and MDM. Proper structuring not only improves clarity but also supports clinical decision-making and billing workflows.
- Review and Approval
- Finally, the generated documentation is presented to the provider for review. At this stage, clinicians can make any necessary edits or corrections. This manual review step ensures accuracy and maintains the provider’s accountability for the patient’s record.
AI scribes streamline documentation, reduce administrative workload, and support more focused patient care. Understanding how these tools function is essential for practices considering the shift to AI-powered solutions.
Benefits of Integrating AI Medical Scribes in Healthcare
AI medical scribes are designed to reduce physician workload and improve the efficiency of clinical practice. By automating documentation, they save time and allow providers to focus more fully on patient care.
These tools also enhance workflow by improving accuracy, standardizing records, and supporting better clinical decisions. Their scalability makes them a strong fit for hospitals, outpatient clinics, and private practices.
Here are some of the key advantages of adopting AI scribes in clinical settings:
- Improves Operational Efficiency and Productivity
One of the most impactful benefits of AI scribes is their ability to streamline physician workflows. Clinicians often spend nearly half of their workday on documentation and entering data into electronic health records. AI scribes help manage this burden by generating real-time transcriptions during patient visits. As a result, providers can spend more time on consultations, patient care, and clinical decision-making.
By completing documentation within the appointment window, these tools reduce after-hours administrative tasks. This supports faster diagnosis, quicker treatment decisions, and a more efficient care delivery process overall.
- Increases Documentation Accuracy
Accurate clinical documentation is essential for effective patient care, proper treatment, and successful billing. AI medical scribes improve accuracy by capturing detailed information as it is spoken, reducing the risk of miscommunication or missed details.
Trained on large datasets and equipped with advanced algorithms, these tools can understand medical terminology and clinical context with a high degree of precision. They help minimize common documentation errors, such as omissions or inconsistencies, and maintain a standardized record of the patient encounter. This consistency supports data integrity across teams and contributes to better long-term care coordination.
- Reduces Physical Burnout
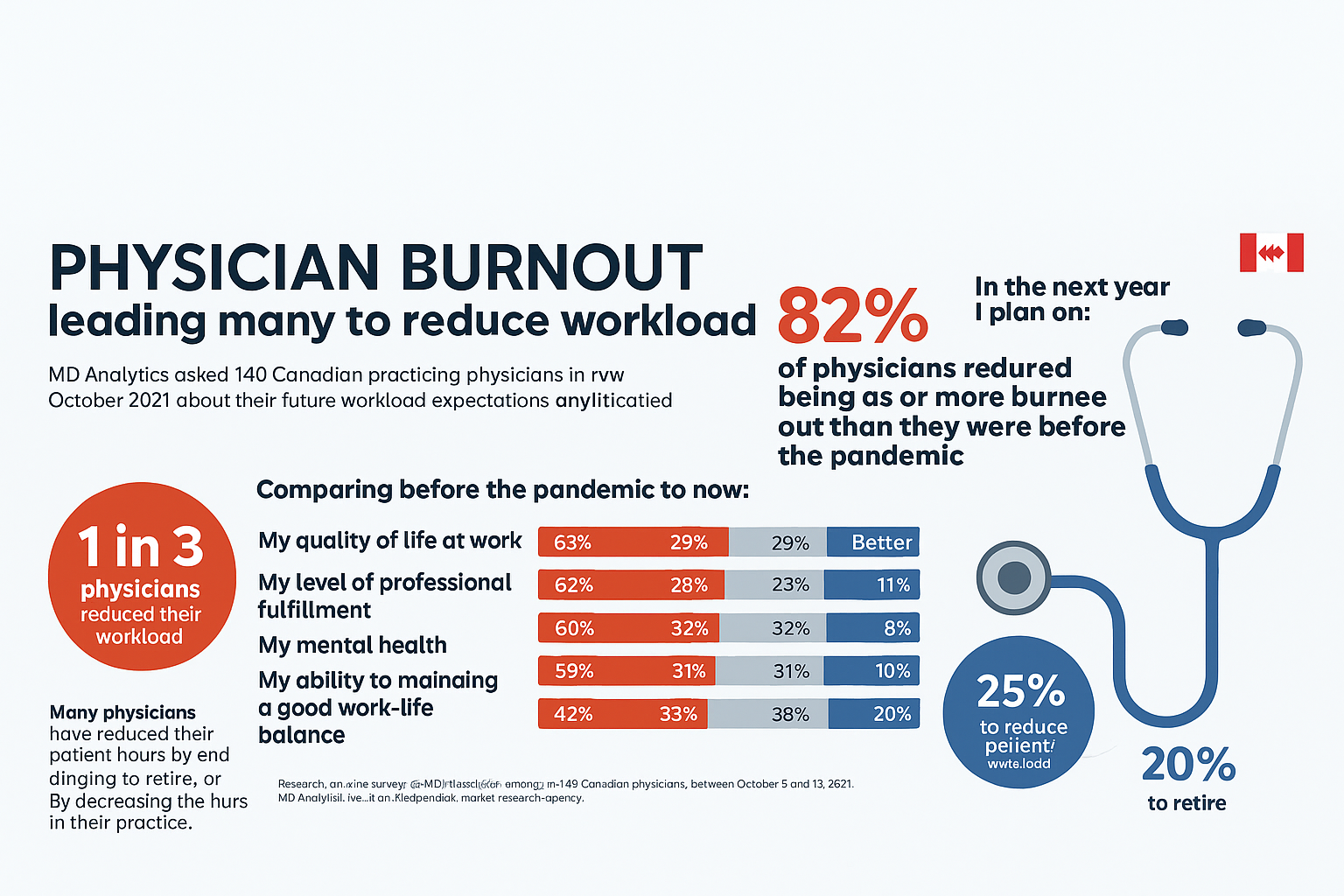
Burnout is a growing concern among healthcare professionals, often driven by increasing administrative workloads. According to national surveys, more than 45 percent of physicians in the United States have reported experiencing at least one symptom of burnout.
AI medical scribes help reduce this burden by taking over much of the repetitive and non-clinical documentation work. This allows clinicians to focus more on patient care and less on after-hours charting, improving work-life balance and supporting mental well-being.
By easing administrative pressure, AI scribes contribute to greater job satisfaction, improved staff retention, and a more engaged clinical workforce. This, in turn, helps boost overall productivity within healthcare organizations.
- Effective Cost Savings
One of the key advantages of using AI scribes in clinical settings is their potential for long-term cost savings. While the upfront investment may appear high, these tools often lead to substantial financial benefits over time.
With a wide range of vendors offering flexible pricing models, practices can choose an option that aligns with their budget and operational needs. Adopting AI scribes reduces the need to hire and manage human scribes, lowering personnel costs. These tools also help prevent billing errors by generating accurate, detailed documentation, which supports cleaner claims and more consistent revenue cycles.
As documentation becomes more efficient, physicians can see more patients within the same timeframe, further contributing to increased revenue and improved practice performance.
- Scalability and Consistency
One of the key strengths of AI medical scribes is their ability to scale across a variety of healthcare environments without compromising documentation quality. From small clinics to large hospitals, these tools provide robust support for automating clinical note-taking and maintaining efficiency as patient volumes grow.
AI scribes promote consistency by enforcing standardized data entry and documentation formats. By ensuring uniform documentation practices, AI scribes help streamline internal processes, improve compliance, and simplify audits.
For organizations aiming to meet regulatory standards and institutional guidelines, AI documentation technologies offer a structured and reliable approach to clinical record keeping. This contributes to better coordination, enhanced accuracy, and more consistent patient care.
Limitations and Challenges of AI Medical Scribes
While AI medical scribes offer numerous benefits, they are not without limitations. Understanding these challenges is important for healthcare organizations considering adoption.
- Contextual Comprehension and Accuracy
- Despite rapid advancements in artificial intelligence, accurately interpreting complex medical context and patient-specific nuances remains a challenge. AI scribes may capture the conversation but still require human review to verify accuracy and ensure clinical relevance.
- Technical Integration
- Although AI scribes are scalable, integrating them with existing electronic health record systems can present compatibility issues. These challenges may affect implementation timelines and limit immediate effectiveness. Over-reliance on digital tools can also pose risks if the software experiences bugs or technical failures, potentially disrupting clinical workflows.
- Data Privacy and Security
- Healthcare organizations manage highly sensitive patient data that must comply with strict privacy regulations. While AI scribes are designed with security in mind, there is growing concern about data privacy risks. It is essential to ensure that any AI solution meets regulatory requirements and implements strong encryption and access control measures.
Final Thoughts
The future of AI medical scribes in healthcare looks promising as technology continues to advance. With ongoing developments in natural language processing and machine learning, these tools are becoming more capable of delivering accurate and context-aware documentation. Automating one of the most time-consuming tasks in clinical practice is a major step toward improving efficiency, reducing burnout, and enhancing productivity.
As AI scribes continue to evolve, their role is expanding beyond basic transcription to become essential tools for streamlining workflows and supporting better patient care. While challenges such as integration, cost, and data privacy remain, the potential benefits make AI scribes a compelling solution for many healthcare organizations.
Integrating AI documentation tools into clinical workflows represents a meaningful shift toward a more efficient and innovation-driven healthcare system. Embracing these technologies can lead to improved outcomes for both providers and patients.
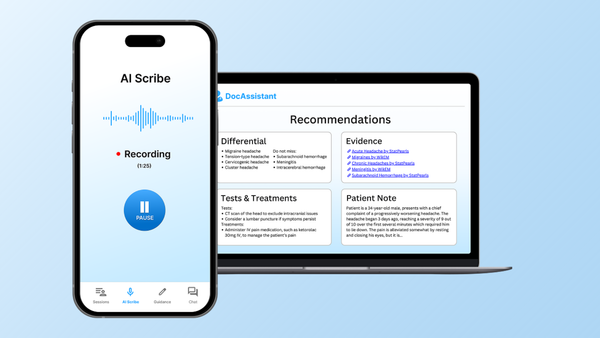
DocAssistant is an industry leading acute care AI Scribe solution that automates clinical documentation using advanced AI scribe capabilities. By capturing real-time interactions between patients and physicians, it generates structured notes that save time and improve accuracy. DocAssistant also offers evidence-based support for clinical decision-making, and a point of care revenue cycle management tool to optimize Emergency Medicine reimbursement.
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline medical documentation and enhance clinical decision making.