How Reimbursement can be Improved & Audit Risk Reduced with AI Solutions

Today’s healthcare professionals have a wide range of responsibilities. In addition to providing high-quality patient care, they must also ensure accurate documentation, compliant billing, and adherence to regulatory standards, all of which can be time-consuming and complex.
Advancements in technology are beginning to ease this burden. AI-powered medical documentation tools and Clinical Decision Support (CDS) systems are reshaping how clinical information is recorded and applied. When used in tandem, these tools help reduce administrative workload, streamline note-taking, support billing accuracy, and assist with timely decision-making.
This article examines how thoughtfully integrating AI tools can support better reimbursement outcomes and reduce audit risk while reinforcing clinical quality and efficiency.
Understanding AI Documentation
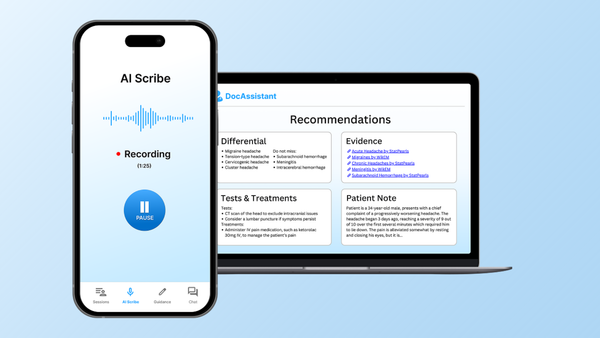
AI-powered documentation tools, often referred to as “AI scribes,” are designed to automatically generate clinical notes. These systems leverage technologies such as natural language processing, machine learning, and automatic speech recognition to capture doctor-patient conversations and convert them into structured documentation.
Traditionally, clinicians would manually enter notes into the Electronic Health Record. In contrast, AI scribes can listen in real time, transcribe spoken language, and format it into standard note types. More advanced solutions may also offer intelligent prompts to enhance compliance and support accurate billing, making them a valuable resource for improving clinical efficiency.
How AI Documentation Works
Medical documentation tools powered by AI integrate several core technologies to function effectively. A foundational component is speech-to-text conversion, which transcribes medical conversations with a high degree of accuracy.
Natural Language Processing then analyzes the transcribed text, identifying key clinical elements, packaging them into a useful note.
By automating the process of clinical note-taking, AI documentation helps reduce administrative burden and supports higher-quality records.
Clinical Decision Support in Practice
Clinical Decision Support systems assist healthcare providers by offering timely, data-driven insights during patient care. By drawing information from the electronic health record and aligning it with clinical guidelines, these tools deliver targeted recommendations, alerts, and reminders that help guide evidence-based decision-making.
Unlike static reference materials, CDS systems are embedded within the clinical workflow. They may alert providers to potential drug interactions, suggest diagnostic tests based on presenting symptoms, or flag overdue preventive screenings.
For example, a CDS system might prompt a physician to order an HbA1c test for a patient with diabetes who has not had one in six months. If a medication is contraindicated due to a patient’s lab values or medical history, the system may recommend a safer alternative.
The primary advantage of CDS lies in its integration with real-time clinical data, enabling more accurate, efficient, and compliant decisions at the point of care.
How AI Clinical Decision Support Works
AI Clinical Decision Support systems help clinicians make informed decisions by combining several advanced technologies. These include rules-based logic, predictive analytics, and machine learning:
1. Rules-Based Engines
These apply established clinical guidelines, such as those from the American Heart Association, to individual patient records. Based on this comparison, the system may highlight potential concerns or suggest relevant actions.
2. Predictive Analytics
By analyzing trends in a patient’s data, predictive tools can estimate future risks, such as hospital readmission or declining kidney function. This allows for earlier intervention and more proactive care.
3. Machine Learning
Here is where the AI comes in- Machine learning enhances adaptability by updating recommendations over time. It draws from historical patient outcomes, population health trends, and ongoing clinical data to refine its guidance.
The Financial Importance of Proper Clinical Documentation
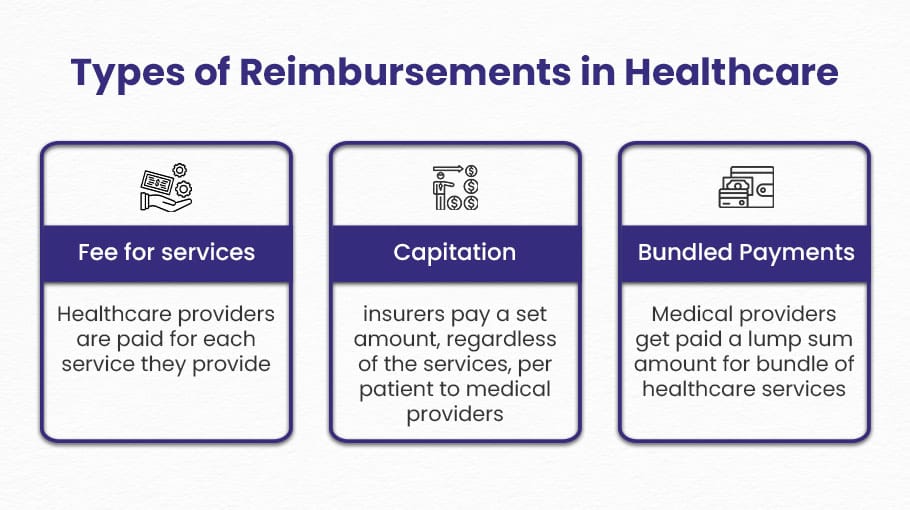
Reimbursement is the process by which healthcare providers are paid for the services they deliver. Accurate and thorough documentation is essential for receiving appropriate payment from both government programs, such as Medicare and Medicaid, and private insurers.
Each diagnosis and treatment must be supported by proper coding, typically involving CPT, ICD-10, and Evaluation and Management (E/M) codes. These codes must accurately reflect the complexity of the visit and the medical necessity of the care provided.
Documentation errors can have significant consequences. Under-coding may result in underpayment, while over-coding can trigger audits and potential legal action. In 2024, the Centers for Medicare & Medicaid Services reported that documentation errors cost the U.S. government $31.7 billion, underscoring the importance of precision in clinical documentation.
Understanding Audit Risk in Healthcare
Audit risk refers to the likelihood that a healthcare provider’s documentation and billing practices will be reviewed by insurers or regulatory bodies. Audits may be triggered by factors such as inconsistent coding, incomplete records, or patterns that deviate from expected norms.
Organizations such as the Centers for Medicare & Medicaid Services (CMS), the Office of Inspector General (OIG), and Unified Program Integrity Contractors (UPICs) are among those responsible for conducting these reviews. When discrepancies are identified, providers may be required to repay funds, face financial penalties, or risk exclusion from payer networks.
As payers increasingly adopt advanced analytics to flag potential issues, maintaining accurate and comprehensive documentation has become critical to reducing audit exposure and ensuring compliance.
How AI Documentation Supports Better Reimbursement
AI-powered medical documentation tools play a key role in improving reimbursement outcomes by ensuring that clinical encounters are accurately and thoroughly documented. They contribute in several important ways:
Accurate Coding
AI scribes help generate clinical notes that clearly support the services being billed. By capturing details such as clinical complexity, time spent, and reviewed symptoms, these tools provide stronger justification for higher-level codes when appropriate.
Reducing Denials
Real-time prompts from AI systems can flag missing or incomplete information. For example, if a patient’s medical history is not documented during a new visit, the AI may prompt the clinician to add it before finalizing the note, helping to prevent claim denials.
Accelerating the Revenue Cycle
AI enables faster documentation, often completing notes by the end of the visit. This allows for quicker billing, reducing the time between service and payment. For smaller practices and Federally Qualified Health Centers, faster billing supports better cash flow and minimizes administrative delays.
In addition, AI helps reduce the need for after-hours documentation, often referred to as “pajama time.” AI scribes help reclaim that time, leading to more complete documentation and decreased clinician burnout.
How Clinical Decision Support Enhances Compliance and Revenue
AI Clinical Decision Support systems do more than aid in clinical decision-making- they also help healthcare providers meet regulatory requirements that directly impact reimbursement, particularly under value-based payment models.
For example, in Medicare’s Merit-Based Incentive Payment System (MIPS), providers are rewarded for reporting and improving outcomes in areas such as diabetes management, cancer screening, and preventive care. CDS tools can help identify care gaps in real time, ensuring that these opportunities are addressed during the patient visit.
In programs like Medicare Advantage, where payment is adjusted based on patient risk, CDS systems play a critical role in accurate documentation. These tools help ensure that chronic conditions are properly recorded, which influences a patient’s Hierarchical Condition Category (HCC) risk score and ultimately affects payment rates. Omitting chronic conditions from documentation can result in substantial lost revenue per patient each year.
CDS platforms with AI capabilities can further enhance this process by analyzing prior notes, lab results, and clinical patterns to confirm or suggest relevant diagnoses, supporting both compliance and revenue integrity.
Reducing Audit Risk with AI and Clinical Decision Support
Audit risk extends beyond financial consequences. It can affect a healthcare organization’s reputation, staff morale, and patient confidence. When audits occur, providers often face increased administrative workload, heightened stress, and decreased productivity.
AI-powered medical documentation tools help mitigate these risks by ensuring that all components of a billable medical encounter are accurately captured and time-stamped. Many systems also include compliance dashboards that flag documentation patterns likely to draw payer attention, such as repeated use of high-level codes without sufficient justification.
Some platforms cross-reference provider notes with payer guidelines and local policies, prompting clinicians to include required details before finalizing documentation. For example, when a high-level service code is used, the system may prompt for thorough documentation of clinical history and decision-making to ensure alignment with coding standards. This reduces the likelihood of coding errors and audit triggers.
Clinical Decision Support tools also contribute by addressing gaps in care that may raise compliance concerns. If a screening or diagnostic test is skipped, the system can require a documented clinical rationale. This level of transparency strengthens the provider’s position during audits and supports defensible, data-backed decision-making.
Navigating Regulatory and Compliance Considerations
While Clinical Decision Support and AI tools offer significant value, their use must align with relevant regulatory frameworks. Certain tools that provide treatment recommendations may be classified as Software as a Medical Device (SaMD) and fall under FDA oversight.
The FDA’s 2022 guidance outlines criteria for determining whether a CDS tool requires regulatory review. In general, if a tool’s logic is transparent and allows the clinician to independently assess and validate its output, it may be exempt from FDA regulation.
When adopting these technologies, healthcare organizations should involve compliance and legal teams early in the procurement process. Ensuring that vendor agreements include appropriate audit provisions and clearly define regulatory responsibilities is essential for long-term risk mitigation and operational readiness.
Future Trends in AI Documentation and Clinical Decision Support
AI in healthcare is rapidly progressing toward more personalized, proactive care. Clinical Decision Support tools are increasingly capable of analyzing complex medical histories and suggesting timely, data-driven insights. Advanced language models, such as GPT-4, are now being used to review patient records, flag critical concerns, and suggest potential diagnoses. In one study, these models demonstrated notable accuracy in identifying digestive conditions, with performance ranging from 40.0 to 91.4 percent depending on the case.
AI-powered documentation tools are also becoming more sophisticated. Many now incorporate ambient intelligence, allowing discreet, real-time recording of doctor-patient conversations through in-room microphones. This reduces the need for physicians to dictate their notes and enables the generation of concise, structured summaries that are ready for review and approval.
As these technologies continue to mature, they are expected to play a greater role in streamlining care delivery, improving documentation quality, and supporting earlier, more precise clinical interventions.
Effective Implementation Strategies
Successful adoption of AI documentation and Clinical Decision Support tools requires a thoughtful, phased approach. Gradual implementation helps ensure clinical workflows remain stable while new systems are integrated.
- Start with a pilot group
Launch with a small group of tech-savvy clinicians to refine processes and gather early feedback.
- Provide comprehensive training
All medical staff should receive clear instruction on how to use the tools, maintain compliance, and communicate feedback.
- Monitor key performance metrics
Track measures such as documentation time, billing code patterns, denial rates, and staff satisfaction to assess the impact.
- Iterate based on real-world use
Continue refining implementation by listening to staff and addressing how the tools affect daily tasks and mental workload.
Ongoing support is essential. Even minor usability issues, such as excessive clicking or frequent screen transitions, can cause frustration in fast-paced environments.
Organizations that emphasize change management and communicate the long-term benefits of these tools, including improved work-life balance and increased revenue, are more likely to achieve lasting success.
Conclusion
AI systems for documentation and Clinical Decision Support have become essential components of modern healthcare. These tools help clinicians complete documentation more efficiently, improve billing accuracy, support safer decision-making, and meet the growing demands of payers and regulators.
When thoughtfully implemented with attention to data quality, fairness, and compliance, these technologies can reduce audit risk, enhance reimbursement outcomes, and contribute to a more sustainable and efficient healthcare system.
One example of a solution designed with these goals in mind is DocAssistant. More than just an AI scribe, DocAssistant offers a comprehensive suite of features that integrate seamlessly into existing workflows and address the full range of challenges from documentation, to clinical decision making, to accurate reimbursement. Try it out today!
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline administrative tasks and enhance clinical decision making.