The Real Cost of Poor Documentation in Emergency Departments

Most emergency department leaders understand that incomplete documentation causes problems. What many don’t realize is just how expensive those problems really are.
The cost of poor documentation extends well beyond denied claims. It shows up in compliance penalties, delayed reimbursements that strain cash flow, and revenue lost when delivered care isn’t accurately captured. For a typical emergency department, these issues can add up to millions in lost revenue every year.
This isn’t about chasing perfection. It’s about recognizing the specific financial and operational consequences of preventable documentation gaps. Emergency medicine presents a uniquely difficult documentation environment consisting of high patient volumes, complex clinical presentations, constant interruptions, and billing requirements that demand precise capture of acuity and procedures.
The impact falls into three core categories:
- Revenue loss from denials and downcoding
- Compliance risk due to audit exposure
- Operational waste from rework and delays
Each one carries a measurable financial burden that many hospital systems continue to underestimate.
Revenue Lost from Denied Claims
Insurance denials related to documentation deficiencies are one of the most visible and costly consequences of incomplete charting. When a claim is rejected because medical necessity is not clearly supported or the documented level of care does not align with the billed code, that revenue is lost unless the appeal process is pursued.
Industry denial rate data shows that 5 to 10 percent of emergency department claims are denied on first submission. In approximately 60 percent of those cases, documentation issues are identified as the primary reason. For a mid-sized emergency department handling 50,000 visits per year with an average reimbursement of $800 per visit, a 6 percent denial rate represents $2.4 million in initially rejected revenue. If documentation gaps account for 60 percent of those denials, that puts $1.44 million at risk due to charting deficiencies.
The average appeal success rate for documentation-related denials is between 50 and 60 percent. This means that roughly half of the denied revenue is never recovered, even after staff invest time and resources in the appeals process. In this scenario, the emergency department would lose between $600,000 and $700,000 in revenue each year from documentation failures alone.
Emergency departments tend to experience higher denial rates than other specialties. This is often due to predictable factors such as complex cases, high volumes, rapid pacing, and fragmented documentation across the patient visit.
Common Documentation Failures That Trigger Denials
Several types of documentation gaps routinely lead to denied claims or reduced reimbursement. These include:
Incomplete encounter narratives
A physician may spend 45 minutes managing a complex case, coordinating a workup, consulting multiple specialists, and making high-stakes clinical decisions. If that effort is not clearly documented, the chart may fail to support the level of service actually provided.
Missing procedure documentation
Procedures such as laceration repairs, joint reductions, incision and drainage, and central line placements often qualify for separate reimbursement. When the indication, technique, or complications are not fully documented, that revenue is lost entirely.
Undocumented critical care time
Charts that lack explicit time tracking or fail to justify the need for critical care often get downcoded to standard evaluation and management levels. This leads to a revenue loss of $200 to $400 per patient.
Vague medical necessity
Generic documentation that could apply to any patient with a similar complaint fails to demonstrate why this particular case warranted emergency evaluation and specific interventions. Without clear justification, claims are more likely to be denied or downcoded.
Compliance Risk and Audit Exposure
Incomplete documentation doesn’t just affect individual claims. It creates serious compliance risks that can lead to penalties far greater than the value of a single chart. CMS and commercial payers regularly audit emergency department billing to look for patterns of upcoding or services that aren’t fully supported by the chart. When documentation issues are widespread, emergency departments face significant financial and regulatory risk.
Office of Inspector General (OIG) reports and work plans have consistently highlighted emergency department evaluation and management billing as a high-risk audit area, with documentation support cited as a frequent concern. When documentation does not clearly support the billed level of service, hospitals may be required to repay the difference. In more serious cases, organizations may face False Claims Act liability or additional enforcement actions.
The financial impact of audits can add up quickly. For example, if upcoding is found in 15 percent of Medicare visits, with an average overbilling of 75 dollars per chart, a 50,000-visit emergency department with 40 percent Medicare volume could owe approximately 225,000 dollars in repayments from a single audit period. If the audit includes multiple years, that total can rise into the millions even before accounting for legal fees or consulting expenses.
The most common compliance vulnerability lies in documenting medical necessity. Payers expect clear, specific justifications for emergency evaluation, ordered tests, and billed levels of care. Vague or templated documentation that could apply to any patient with a similar complaint does not meet that threshold and increases audit risk.
Emergency medicine billing guidelines require documentation that reflects the complexity of medical decision-making used to justify the evaluation and management level. This means showing the differential diagnoses considered, the data reviewed, the patient’s level of risk, and the uncertainty involved in clinical decisions. Charts that only include a diagnosis and treatment plan, without explaining the reasoning behind those choices, are especially vulnerable to downcoding during audits.
The cost of compliance risk extends beyond financial penalties. Audits create operational disruption as staff are pulled from their daily responsibilities to retrieve charts, respond to documentation requests, and implement corrective action plans. Legal and consulting fees for audit support can quickly reach six figures. Compliance issues may also damage a hospital’s reputation, potentially affecting payer negotiations and straining relationships with employed physicians.
Revenue cycle teams invest significant time and resources into preventing compliance issues through pre-bill audits and ongoing physician education. When documentation quality is inconsistent, this effort becomes a costly defensive strategy - reviewing charts, issuing physician queries, and holding claims to avoid submitting non-compliant documentation. While these efforts may not appear as direct line items, they represent substantial staffing costs and lost opportunities elsewhere in the organization.
Operational Costs
Poor documentation leads to operational inefficiencies that surface in several ways. Physicians spend time responding to coding queries about incomplete charts. Revenue cycle staff dedicate hours reviewing documentation and requesting clarifications. Reimbursement is delayed as charts are corrected and claims are resubmitted. These costs are less visible than denied claims but can be just as significant.
The average emergency physician receives three to five coding queries per week related to documentation gaps or ambiguities. Each query requires the physician to review the chart, recall the patient encounter, and respond with clarifications or addenda. At 10 to 15 minutes per query, this adds up to 30 to 75 minutes of uncompensated time each week. In a 12-physician department, that translates to 6 to 15 hours weekly spent on rework.
Valuing physician time at a conservative $200 per hour, a department spending 10 hours per week on documentation queries incurs $104,000 annually in physician time spent fixing avoidable issues. This does not account for the added frustration and burnout caused by repeated rework.
Revenue cycle staff face similar challenges. Medical coders and health information management professionals often spend a significant portion of their time reviewing charts, identifying gaps, and following up with physicians. When documentation is consistently poor, this becomes their primary focus rather than higher-value activities like denial prevention and compliance monitoring.
Documentation delays also have a real impact on cash flow. Claims that cannot be submitted due to missing or unclear information are held in pending status, often for weeks. For hospitals operating on tight margins, this creates financial strain. A 30-day delay in billing just 10 percent of emergency department volume can result in millions of dollars in delayed revenue for larger systems.
There are also risks to care coordination and patient safety. When documentation does not clearly communicate the emergency department’s evaluation and treatment plan, downstream providers may lack essential context. This can lead to duplicate testing, missed follow-up, or incomplete treatment - each carrying quality, liability, and financial consequences.
Physician satisfaction and retention are also at stake. Documentation burden is a top driver of burnout among emergency physicians. When poor documentation practices lead to constant queries and rework, dissatisfaction grows. Replacing just one emergency physician costs between $250,000 and $500,000 in recruiting, onboarding, and lost productivity. If poor documentation contributes to even a single physician departure every few years, the resulting cost is substantial.
What Good Documentation Actually Looks Like in Emergency Departments
High-quality emergency department documentation meets several specific criteria that directly address the failure points discussed earlier. These standards are not about perfection, but about consistency, clarity, and alignment with compliance and billing requirements.
Essential elements of compliant emergency department documentation include:
Complete Real-Time Capture
The history of present illness includes relevant positives and negatives. The physical exam covers all pertinent systems. Medical decision-making reflects the full clinical picture by outlining differential diagnoses, reviewing supporting data, and documenting risk assessment.
Billing-Level Alignment
The documented care clearly supports the evaluation and management level billed. High-complexity visits reflect that complexity through the number and severity of conditions addressed, the extent of data reviewed, or the risk associated with the patient’s condition.
Patient-Specific Medical Necessity
Documentation explains why this particular patient required emergency evaluation and why each test or treatment was appropriate. It avoids vague or templated phrasing in favor of details unique to the encounter.
Audit Defensibility
The chart presents a logical, coherent clinical narrative that would make sense to an auditor or third-party reviewer assessing the medical necessity of decisions and services provided.
Procedure Completeness
All procedures are documented with clear indication, technique, findings, and any complications, supporting accurate coding and payment.
Precise Critical Care Documentation
Start and stop times are included, along with a clear rationale for why the patient met the threshold for critical care services.
Most emergency departments struggle to consistently meet these standards because doing so demands significant physician time and attention during already demanding shifts. Physicians often manage several patients at once, respond to new arrivals, and handle high-acuity situations. As a result, detailed documentation is frequently deferred until the end of the shift, when fatigue sets in and memory fades.
Traditional solutions like documentation training and templated notes provide partial support but fail to resolve the core challenge. Templates can help with structural completeness but often lead to overly generic charts that fall short of establishing medical necessity. Training raises awareness of what is required but does not give physicians more time during their shifts to meet those expectations.
The emergency department workflow presents documentation challenges that are distinct from those faced by other specialties. Constant interruptions make real-time note-taking difficult. Physicians must shift attention rapidly between cases, which increases the risk of missing documentation elements. In high-acuity situations, documentation becomes a secondary priority, often postponed until the end of the shift when energy and attention are lowest.
The Cost of Doing Nothing
The cumulative impact of poor documentation(across denied revenue, compliance risk, and operational inefficiency) easily surpasses $500,000 annually for a typical emergency department handling 50,000 visits. In higher-acuity or larger facilities, the total often climbs into the millions.
Consider the breakdown: $600,000 in denied claims, $100,000 in physician time spent on documentation queries, $150,000 in revenue cycle rework, and additional exposure from compliance audits. This doesn’t include the hidden financial drag from delayed reimbursements, physician burnout, and turnover. Nor does it reflect the opportunity cost of time spent addressing documentation issues instead of investing in quality initiatives or patient experience improvements.
The return on investment for solving this problem is clear. Solutions that enable emergency physicians to document care accurately and completely directly reduce costs in all three categories. Revenue capture improves when procedures and complexity are properly documented. Compliance risk decreases when documentation meets payer expectations for medical necessity and code justification. Operational efficiency improves as queries decline and billing cycles shorten.
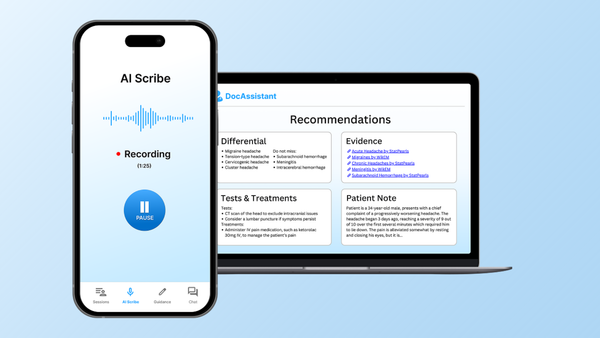
Emergency medicine-specific documentation tools provide unique value because they align with the pace, pressures, and workflows of the emergency department. The most effective tools do more than transcribe dictation. They support real-time clinical thinking and guide documentation toward billing and compliance standards.
For instance, if a physician spends extended time managing a complex case, a well-designed tool will prompt for critical care documentation. If clinical decision rules are applied, the tool ensures that supporting details are captured appropriately. These seemingly small interventions translate to major financial gains.
Case studies of AI-powered documentation tools built for emergency medicine demonstrate this clearly. Emergency departments using these systems report an average of $399,000 in additional annual revenue per physician - primarily through better capture of evaluation and management levels, procedural documentation, and critical care time. This revenue is not newly generated. It is revenue that would otherwise be missed due to documentation gaps.
How to move forward
The cost of poor documentation in emergency departments is both measurable and substantial. Revenue lost to denials, penalties from audits, and operational inefficiencies caused by documentation rework often total millions of dollars each year.
Addressing this challenge requires more than transcription tools. It calls for solutions built specifically for emergency medicine. These tools must understand real clinical workflows and actively support the creation of complete, compliant documentation. The difference between adequate and excellent documentation has direct consequences for hospital financial performance, operational efficiency, and physician well-being.
Emergency departments that take the time to quantify their current documentation costs and compare them to the investment in a specialized solution often find a clear and compelling return on investment. The real question is no longer whether poor documentation is costing your organization. It is. The better question is whether the tool you are considering directly addresses the core workflow, compliance, and billing challenges unique to emergency medicine.
Ready to understand your emergency department's specific documentation cost profile? Schedule a documentation assessment to identify revenue leakage and pinpoint where incomplete documentation is impacting performance. You can also review case studies that highlight the measurable financial gains achieved with emergency medicine-specific documentation solutions.
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline medical documentation and enhance clinical decision making.