Choosing the Best AI Scribe for Emergency Medicine in 2025
In this guide, we'll examine the current AI scribe landscape, analyze why popular platforms struggle in emergency medicine environments, and explore the key factors you should consider when evaluating documentation tools for the ER.

Finding the best AI scribe for emergency medicine isn’t about choosing the most popular platform, it’s about finding one built for the chaos of the ER. Unlike primary care, emergency physicians can find themselves managing 8+ patients at once, make life-or-death decisions in minutes, and need documentation that captures complex clinical reasoning without slowing them down.
In this guide, we'll examine the current AI scribe landscape, analyze why popular platforms struggle in emergency medicine environments, and explore the key factors you should consider when evaluating documentation tools for the ER. In closing, we'll also share a little about DocAssistant, our AI scribe built specifically for emergency and acute care physicians.
The Emergency Medicine Documentation Challenge
Emergency medicine operates differently from other medical specialties in ways that affect documentation requirements:
Multi-patient management: Emergency physicians typically oversee many patients simultaneously across varying acuity levels, creating documentation complexity that doesn't exist in scheduled, single-patient encounters.
Time-critical decision making: Clinical decisions often occur within minutes, with limited opportunity for real-time documentation of the reasoning process.
Undifferentiated complaints: Patients present with symptoms rather than diagnoses, requiring systematic evaluation and documentation of multiple potential conditions.
Complex differential diagnosis: Emergency physicians must systematically exclude multiple life-threatening conditions for seemingly simple complaints, requiring sophisticated clinical reasoning that's difficult to capture quickly.
Regulatory scrutiny: Emergency departments face intense oversight from payers and quality organizations, demanding documentation that withstands rigorous review.
These factors create documentation needs that differ significantly from primary care or specialty clinic workflows.
Current Dictation and AI Scribe Landscape
Several documentation solutions are popular among emergency medicine physicians, each with different strengths and limitations:
Dragon Medical One - Well-integrated with many EHR systems, good for dictation-style documentation, though requires significant training to use effectively. The traditional dictation model struggles in emergency medicine's multi-patient environment where physicians frequently switch contexts mid-sentence.
Nuance DAX (now Microsoft) - Uses conversational AI to capture patient encounters and works well for natural documentation flow with Epic and other major EHRs. However, DAX was designed around scheduled encounters with predictable conversation flow, making it less effective when emergency physicians are managing multiple critical patients simultaneously. This product can also be cost prohibitive.
Abridge - Specifically designed for clinical conversations, creates structured notes from patient interactions, and is gaining traction across various specialties. While Abridge shows promise in emergency medicine, it wasn't built specifically for ED workflows and can struggle with the rapid context switching that defines emergency medicine and underdelivers in the MDM- the meat and potatoes of the Emergency Medicine documentation.
Suki AI - Voice-enabled assistant that works across different EHR platforms, designed to reduce documentation burden through voice commands. Suki's voice-first approach can work well for single-patient encounters, but emergency physicians report losing clinical context when managing multiple critical patients where conversations frequently overlap.
Augmedix - Combines AI with human oversight, providing real-time documentation support during patient encounters. While the hybrid model offers quality assurance, the human element adds cost and can create delays that don't align with emergency medicine's time-critical workflows.
The Primary Care Adaptation Problem
All the platforms above have gained significant adoption across medicine, but most were developed primarily for primary care and specialty clinic environments. They excel at:
- Converting patient-physician conversations into structured notes
- Working within scheduled appointment frameworks
- Supporting single-patient, one touch encounters
- Integrating with common EHR systems
Their primary care origins create fundamental limitations in emergency medicine settings. When you're called away from documenting a chest pain patient to intubate a trauma patient, then return to discharge the original patient, these platforms struggle to maintain clinical context and often mix elements between encounters.
Key Evaluation Criteria for Emergency Medicine
Workflow Compatibility
Multi-patient context management: Can the system maintain separate documentation streams when you're managing multiple patients simultaneously? Most platforms lose track when you switch between a chest pain workup, a pediatric fever, and a psychiatric evaluation within the same conversation thread.
Interruption handling: Emergency medicine involves constant interruptions for codes, traumas, and critical decisions. How effectively does the platform resume documentation after you're called away mid-encounter for a life-threatening emergency?
Acuity variation: Does the system adapt to different encounter types, from minor complaints requiring simple documentation to complex resuscitations demanding detailed critical care notes?
Multiple touch points: The largest difference between documenting in the ER and in primary care is that in the ER a doctor might need to update the chart 2, 3, 4, and sometimes even more times. In the primary care clinic the conversation can usually be accomplished in one physician patient conversation. This requires a different user interface for an AI Scribe.
Emergency Medicine-Specific Clinical Intelligence
Clinical decision rules: Can the platform recognize and document when you use emergency medicine-specific tools like HEART score for chest pain, PERC rule for pulmonary embolism, or the ICH score for intracranial hemorrhage.
Knowledge base integration: Does it connect with emergency medicine resources like WikiEM for protocols, StatPearls for evidence-based databases for complex management of critical patients?
Multi-system evaluation: Emergency physicians don't treat specific diseases - they evaluate undifferentiated complaints that could represent multiple conditions across different organ systems. Can the platform document this systematic approach?
Revenue Recovery and Compliance
Emergency medicine billing involves specific complexities around evaluation and management levels, critical care documentation, and procedure integration. Can the platform identify and document:
- External medical records review
- Risk stratification methodology
- Consultant coordination activities
- Complex medical decision-making processes
- Multi-system evaluation components
Building an AI Scribe for the ED
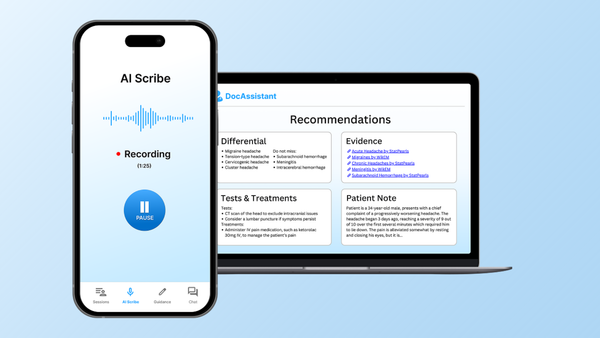
DocAssistant was founded by Dr. Nathan Murray, a practicing emergency medicine physician who experienced firsthand the limitations of generic AI scribes in emergency department workflows. Rather than adapting a primary care tool, DocAssistant is designed specifically around emergency medicine's unique requirements:
Multi-patient management: DocAssistant maintains separate conversation threads for multiple patients simultaneously. When you're called away from one patient for an emergency, the system preserves context and seamlessly resumes documentation without mixing clinical elements between encounters.
Emergency medicine clinical intelligence: The platform integrates with WikiEM and StatPearls, providing real-time access to emergency medicine protocols and evidence-based recommendations. When you mention using clinical decision rules, the system understands these tools and documents them appropriately.
Revenue cycle integration: Unlike transcription-only tools, DocAssistant analyzes each encounter for billing implications, identifying elements like external records review, risk assessment tool utilization, and complex medical decision-making processes that are routine in emergency medicine but often missed by generic platforms.
Clinical Validation in Real Emergency Medicine Settings
DocAssistant's effectiveness has been demonstrated in actual emergency medicine environments. Elite Hospital Partners implemented the platform in their emergency department and documented substantial outcomes:
- Emergency physicians captured an additional $33,264/month in additional reimbursement per physician through more complete documentation of care already provided
- Documentation time decreased by 85%, eliminating most after-hours charting
- Zero billing rejections due to AI-generated notes
- Maintained normal patient throughput while significantly improving documentation quality and compliance
Real Emergency Physician Feedback
Reviews of DocAssistant show it delivers what generic AI scribes can't: documentation that actually works in the ED's chaos.
The impact on physician burnout is immediate. Allan J. went from being "bogged down with charts on the regular" to getting "to rest on my days off instead of trying to catch up on charts." Christian P. found he could "see more volume than my peers" while never leaving "a shift with incomplete notes"—exactly what emergency physicians need when managing multiple critical patients.
Dr. Andrea G. notes DocAssistant "provides a thorough diagnostic differential tailored to my patient's complaints," while a Level 1 trauma center physician calls it "incredibly helpful to have a tool that allows me to be efficient and effective on shift." This systematic clinical reasoning support is what separates purpose-built emergency medicine tools from generic transcription platforms.
Multiple physicians describe the platform as "a lifesaver" and "a game changer."
Testing and Implementing an AI Scribe
Pilot Testing
Given the high stakes of emergency medicine documentation, thorough evaluation is essential. Consider testing platforms during different scenarios:
- High-volume periods with multiple simultaneous patients
- Critical care scenarios requiring detailed documentation
- Complex cases involving multiple consultants and procedures
Integration Requirements
Emergency medicine AI scribes must work within existing ED workflows:
- EHR compatibility with emergency medicine templates
- Bed management system coordination
- Mobile device functionality for bedside documentation
- Compatibility with existing quality assurance processes
Measuring Success
Success should be measured across multiple dimensions:
- Documentation completeness and accuracy
- Time to complete notes
- Billing compliance and revenue optimization
- Physician satisfaction and adoption rates
The Future of Emergency Medicine Documentation
Emergency physicians need an AI scribe and documentation tool built for their reality: managing multiple patients at once, making split-second decisions, and capturing complex clinical reasoning under relentless time pressure.
That's why we created DocAssistant, purpose-built by emergency physicians, clinically validated in high-volume ERs, and proven to recover revenue, cut charting time, and restore work-life balance.
Ready to transform your emergency medicine documentation? Experience the difference a purpose-built AI scribe makes in your workflow.
Try DocAssistant Free | Download iOS App | Download Android App