What to look for in AI scribe tools

In today’s fast-paced healthcare environment, clinicians are expected to see more patients, handle less paperwork, and still deliver high quality care while managing stress and avoiding burnout. That is where AI medical scribes come in. These digital tools automatically capture and organize clinical notes, easing the documentation burden.
As AI scribes become more common in 2025, choosing the right one is more important than ever. Whether you are a solo provider, part of a hospital system, or running a specialty clinic, this guide covers the must have features and compares five leading options to help you make the right choice.
Why AI Medical Scribes Are Essential in 2025
In 2025, healthcare professionals face increasing pressure. They are expected to see more patients, keep up with shifting regulations, and still deliver high-quality care. Much of their time is spent on documentation instead of patient interaction.
Studies show doctors often spend nearly twice as much time on electronic records as they do with patients. This imbalance adds to stress and burnout.
AI medical scribes solve this by automating clinical documentation. They listen to patient visits and generate structured notes in real time. This reduces errors, saves time, and improves note quality. Instead of finishing charts late at night, clinicians can rely on AI to capture accurate details during or immediately after each visit.
These tools also support proper coding and documentation standards. By improving accuracy, they help reduce claim denials and the risk of audits. Leading AI scribes now understand context, refer to patient history, and adapt to different specialties. They also work well in both in-person and virtual care.
The result is less time on paperwork, more meaningful patient care, and higher productivity. In today’s fast-paced healthcare environment, AI scribes are no longer optional. They are becoming essential.
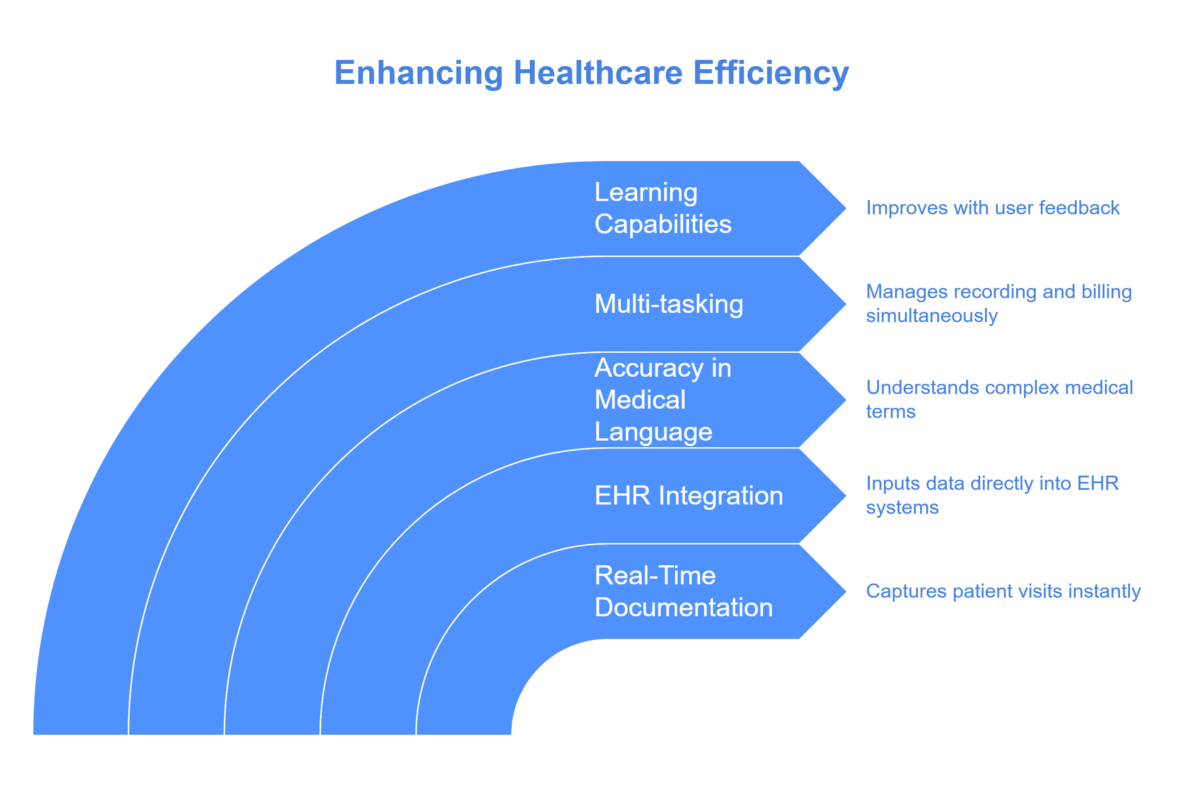
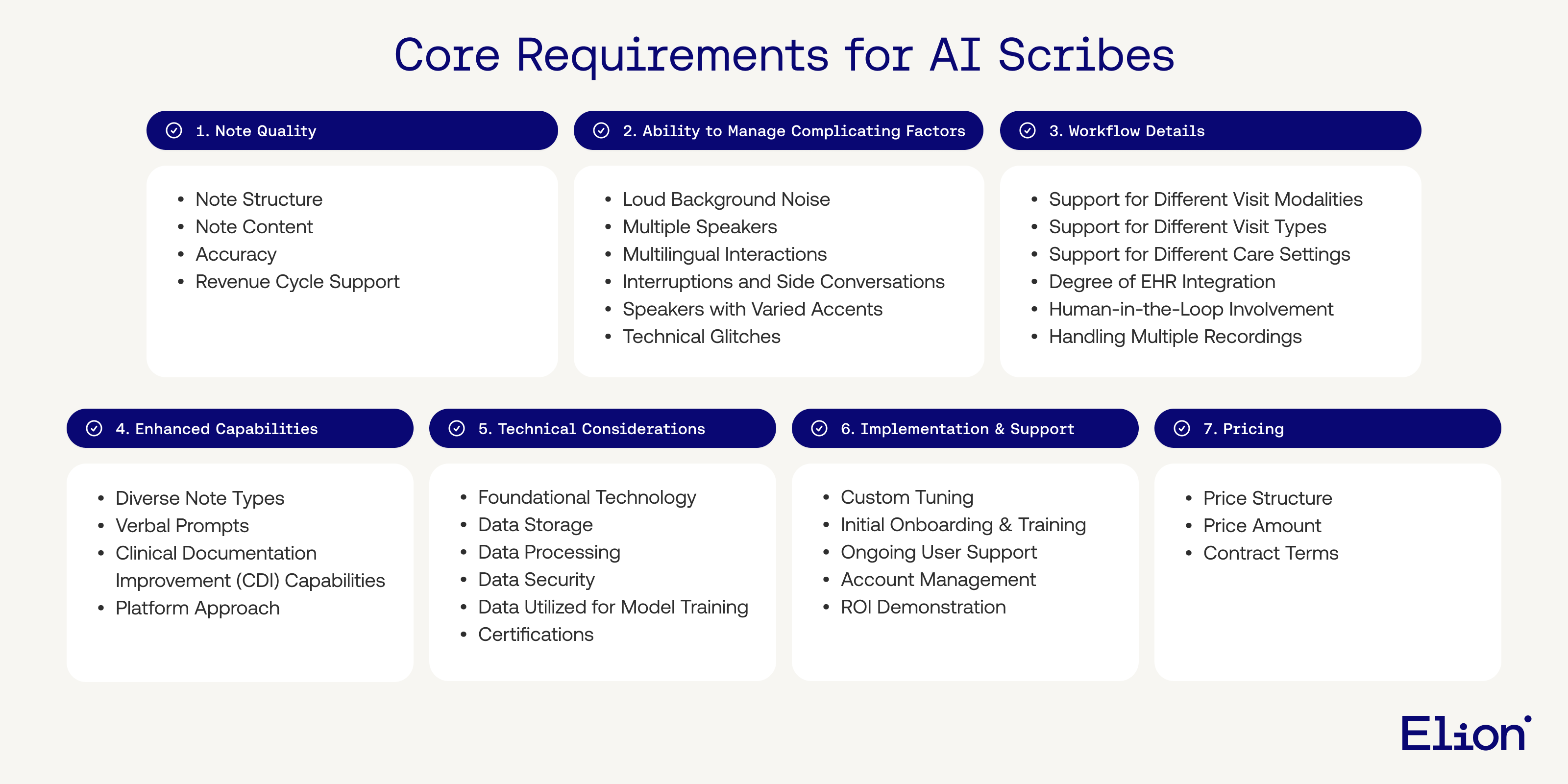
Key Features to Look For
- Accuracy and Real-Time Transcription
A strong AI scribe converts spoken words into written text with high accuracy. It should perform well even with background noise, different accents, and complex medical terms. Real-time transcription allows providers to quickly verify notes and catch important details on the spot. Errors in transcription can disrupt workflow and lead to patient safety or billing issues.
- EHR Integration
The AI scribe must connect smoothly with your current Electronic Health Record system. This reduces duplicate entry and ensures smooth operations. Proper integration means syncing charts and data fields correctly. Poor EHR compatibility can frustrate providers and slow down care. A well-integrated scribe improves satisfaction and supports a more efficient workflow.
- HIPAA Compliance
Protecting patient information is a legal and ethical responsibility. AI scribes must meet HIPAA requirements. Look for features such as encryption, access controls, and audit logs that protect electronic health information.
- SOAP Note Generation
A quality AI scribe produces structured SOAP notes that are easy to review. These notes support continuity of care, ease audits, and promote consistent documentation. Automating this process reduces manual input while still allowing provider oversight.
- Customization and Adaptability
Each medical practice has unique needs. AI scribes should offer custom templates and allow adjustments for different specialties. Tailoring voice commands and note formats improves adoption and makes documentation faster.
- Multi-Speaker Support
Medical visits often involve multiple people like doctors, nurses, and family members. An effective scribe should distinguish speakers to keep notes clear. This is especially important in team-based care where mixing up speakers can cause confusion.
- Use of Patient History
Advanced AI scribes can reference prior records to make notes more insightful. Access to lab results, medication history, and chronic conditions helps improve care decisions and documentation quality.
- Multilingual Support
Language access matters. About 25 million people in the U.S. are not confident in English. AI scribes that understand multiple languages and dialects can improve equity, accuracy, and patient satisfaction.
- Telehealth Compatibility
With more care delivered through telehealth, AI scribes should work well during video or phone visits. Integration with platforms like Zoom or Teams ensures consistent documentation across care settings.
- Flexible Workflows
AI scribes should support different work styles. That includes mobile access, batch documentation, and options for both real-time and post-visit transcription. Tools designed with clinician feedback in mind will be more successful in the long run.
How to Select the Best AI Scribe
- Identify Your Issues
Start by pinpointing your specific challenges. Are you dealing with after-hours documentation? Do you lack tools for telehealth? Knowing your pain points helps you choose a scribe that directly solves them.
- Focus on Key Features
Once your needs are clear, prioritize the features that matter most. If your practice relies on remote care, telehealth compatibility is essential. Specialty clinics may need custom templates. Align features with your goals to avoid overspending on extras you will not use.
- Compare Different Solutions
Look at tools side by side to weigh their strengths and limitations. Use third-party reviews and independent studies to guide your decision. Comparing options helps you find the best match for your workflow and budget.
- Check System Integration
Make sure the scribe connects smoothly with your electronic health records, scheduling tools, and telehealth platforms. Strong integration saves time and reduces errors. Look for support for APIs and widely used standards like FHIR and HL7.
- Try Before Deciding
Always test the product through live demos or trials. This shows how the tool performs in your day-to-day setting. Try it out with real patient visits to gauge accuracy and usability. Choosing a tool you have tested boosts your chances of long-term success.
The Value of Investing in the Right AI Scribe
Choosing an AI medical scribe is more than a technology upgrade. It is a strategic step that reshapes clinical workflows. The right AI tool reduces time spent on documentation, improves job satisfaction for doctors and nurses, and enhances both patient outcomes and financial results. When clinicians spend less time writing notes and more time with patients, the quality of care improves. This can lead to better health results, higher patient loyalty, and improved satisfaction scores.
From a financial standpoint, fewer documentation errors mean more accurate billing and fewer claim denials. This helps ensure proper reimbursement. For overwhelmed staff, AI scribes lighten the load and support long-term retention. Modern AI scribes are built for flexibility. They work well in solo practices, large hospital systems, and hybrid care models.
Choosing a medical scribe that fits your workflow, technology stack, and specialty sets the foundation for long-term success. These tools do more than simplify paperwork. They help improve care and elevate the healthcare experience.
Top AI Medical Scribe Options for 2025
Here are some of the leading AI scribe tools available today, listed in alphabetical order. Each offers unique strengths and capabilities to support different clinical workflows.
- DeepScribe
Best for: Clinicians who want fully automated documentation with high accuracy
Why it stands out:
DeepScribe listens to doctor-patient conversations in real time and automatically generates complete clinical notes. This makes it a strong choice for busy clinics looking to save time without compromising accuracy.
Key Features
- Ambient listening with automatic note creation
- Connects with both hospital and outpatient electronic health records
- Secure and compliant with HIPAA regulations
- Requires minimal input from clinicians
- Notes can be reviewed and edited before finalization
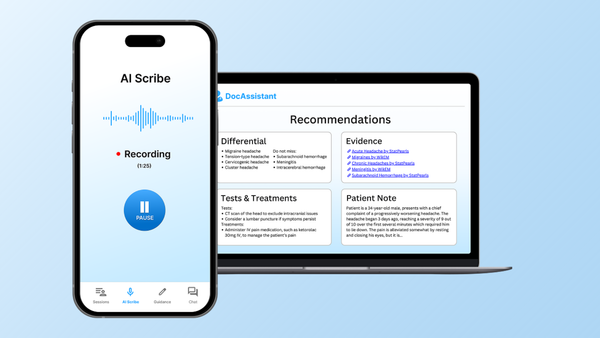
- DocAssistant
Best for: Practices that need reliable real-time transcription with strong customization options
Why it stands out:
DocAssistant delivers highly accurate transcription while incorporating a deep understanding of patient history. It generates complete clinical notes efficiently and fits smoothly into existing workflows.
Key Features
- Real-time documentation
- Full integration with electronic health records
- Built-in privacy and security safeguards
- Compatible with telehealth and phone consultations
- Flexible workflows with pause, resume, and batch support
- Access to past patient records
- Voice command support and specialty-specific templates
- Multilingual transcription capabilities
- Freed
Best for: Clinicians who value simplicity and ease of use
Why it stands out:
Freed focuses on a streamlined experience, making it a great choice for solo practitioners or small clinics aiming to reduce time spent on documentation without dealing with complexity.
Key Features
- Hands-free real-time scribing
- Simple and intuitive to use
- Integrates with major electronic health records
- Produces structured clinical notes
- Mobile and user-friendly interface
- Strong customer support
4. Heidi
Best for: Allied health professionals and multidisciplinary teams
Why it stands out:
Heidi is built to serve more than just physicians. It supports professionals like nurses, dietitians, therapists, and veterinarians. Its flexible language and design adapt to various workflows and clinical roles.
Key Features
- Tailors language and terms to each profession
- Offers customizable templates for different specialties
- Manages multi-speaker team conversations
- Allows easy review and structured note export
- Integrates with a wide range of non-hospital electronic health records
5. MarianaAI
Best for: High-volume practices that need efficient chart management
Why it stands out:
MarianaAI is designed to handle scale. It offers chart summarization, accurate patient identification, and customizable templates, making it ideal for teams managing a large number of clinical notes each day.
Key Features
- Handles large volumes of charts without slowing down
- Uses AI to match patient IDs and notes accurately
- Creates complete SOAP notes
- Integrates with complex and specialized workflows
- Prioritizes data privacy and regulatory compliance
Final Thoughts
AI medical scribes are evolving quickly. By 2025, there will be more options than ever, each offering different strengths. The key is to find a tool that fits your workflow, supports your documentation needs, and integrates well with your existing systems. When chosen thoughtfully, an AI scribe can boost provider satisfaction, reduce administrative burden, and improve both care quality and financial performance.
DocAssistant is one of the tools leading this shift. With strong EHR integration, real-time SOAP note generation, and support for various specialties, it is built to meet the needs of modern healthcare teams. Its focus on compliance and ease of use makes it a valuable option for practices looking to work more efficiently and spend more time with patients.
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline medical documentation and enhance clinical decision making.