
The Real Cost of Poor Documentation in Emergency Departments

Artificial intelligence has entered many industries, including healthcare. In medicine, AI helps improve accuracy, enhance patient safety, reduce workload, and support faster clinical decisions. It is also becoming increasingly important in managing administrative tasks. In the fast-paced environment of the emergency department, these capabilities are especially valuable for improving patient
Clinician-Built AI Scribe Platform Demonstrates Year-Long Commitment to Industry-Leading Security Standards San Diego, California – January 3rd, 2025 – DocAssistant, the comprehensive AI-powered scribe, clinical decision support, and point-of-care RCM solution designed specifically for Emergency Departments and Hospitalists, today announced it has successfully achieved SOC 2 Type 2 certification. This milestone underscores
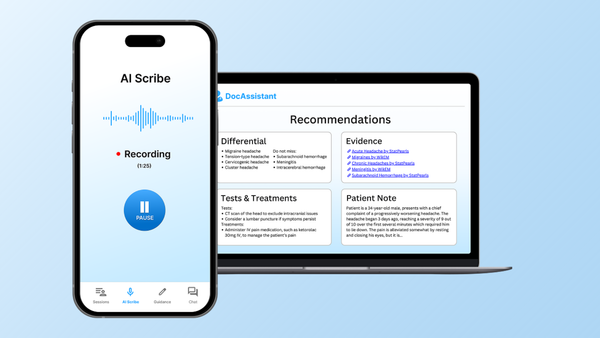
Elite Hospital Partners found that their Emergency Medicine physicians that used DocAssistant's HIPAA-compliant AI scribe and Clinical Decision Support Tool reduced charting time by 85% while capturing an average of $399,168 in additional annualized revenue per physician through more complete clinical documentation. "Emergency physicians spend way

Background Elite Hospital Partners partnered with DocAssistant to evaluate the financial and operational impact of AI-generated clinical documentation in the emergency department. Objective The core objective was to improve physician documentation quality in alignment with the 2023 CMS Evaluation & Management (E/M) guidelines, thereby capturing the full value of

In this guide, we'll examine the current AI scribe landscape, analyze why popular platforms struggle in emergency medicine environments, and explore the key factors you should consider when evaluating documentation tools for the ER.

Imagine walking into your clinic and being met not by a stack of paperwork, but by the opportunity to focus more fully on your patients. Research shows that clinicians now spend more time documenting than engaging with those they care for (Ammenwerth and Spötl, 2009). This growing challenge has sparked
In today’s fast-paced healthcare environment, clinicians are expected to see more patients, handle less paperwork, and still deliver high quality care while managing stress and avoiding burnout. That is where AI medical scribes come in. These digital tools automatically capture and organize clinical notes, easing the documentation burden. As

Believe it or not, the scribe profession dates back thousands of years, nearly as far as the invention of writing itself. Historians note that scribes in ancient Egypt and Mesopotamia were highly educated individuals responsible for recording events and managing administrative duties. These scribes often belonged to the upper tiers

Electronic Health Records are now a core part of modern healthcare, used by more than 90 percent of hospitals and nearly 90 percent of private practice physicians in the United States, as of 2021. These systems make it easier to store and access patient information, improving the organization of medical

The healthcare industry is undergoing a major transformation, driven by rapid advancements in technology. Among the most impactful innovations is the emergence of AI medical scribes, digital tools designed to streamline clinical documentation and reduce the administrative burden on physicians. These systems are reshaping how medical professionals manage patient records,

In today’s healthcare environment, physicians are responsible for much more than diagnosing and treating patients. A substantial portion of their time is spent entering information into Electronic Health Records. Research shows that many doctors now spend more time on documentation than with patients, contributing to dissatisfaction and burnout. To