AI-Powered Clinical Decision Support: How It’s Changing Patient Outcomes in 2025

Imagine being part of a world where you have a virtual assistant at your disposal - one equipped with up to date medical knowledge to guide you when assessing patients. Sounds far-fetched? Well, it is not! This is precisely what is now known as Clinical Decision Support or CDS. It refers to a computer program that aids healthcare professionals in making better decisions at work.
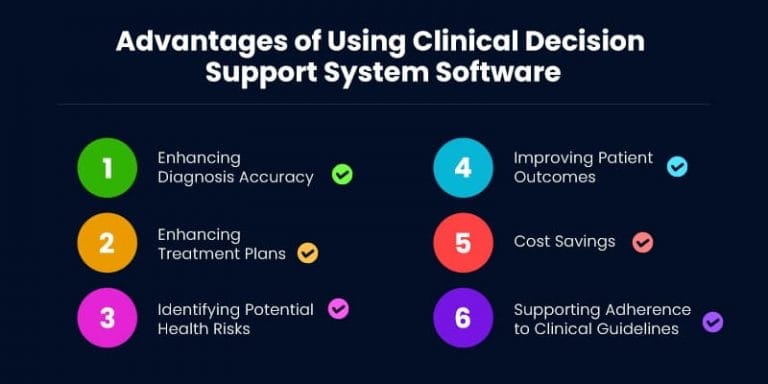
CDS is a pivotal advancement in healthcare. It makes use of its technological data and medical expertise to come up with actionable insights and evidence-based recommendations. It has thus significantly heightened diagnostic accuracy, treatment efficacy, and overall improved patient outcomes.
CDS serves as a cognitive aid, helping clinicians in navigating the challenges of modern medicine. The tool/software analyzes patient data, medical literature, and medical best practices to come up with tailored suggestions and alerts. CDS is making its inroads across the globe because of its ability to mitigate diagnostic errors, bring down healthcare costs, optimize treatment plans, and improve the overall quality of patient care.
The growing role of AI
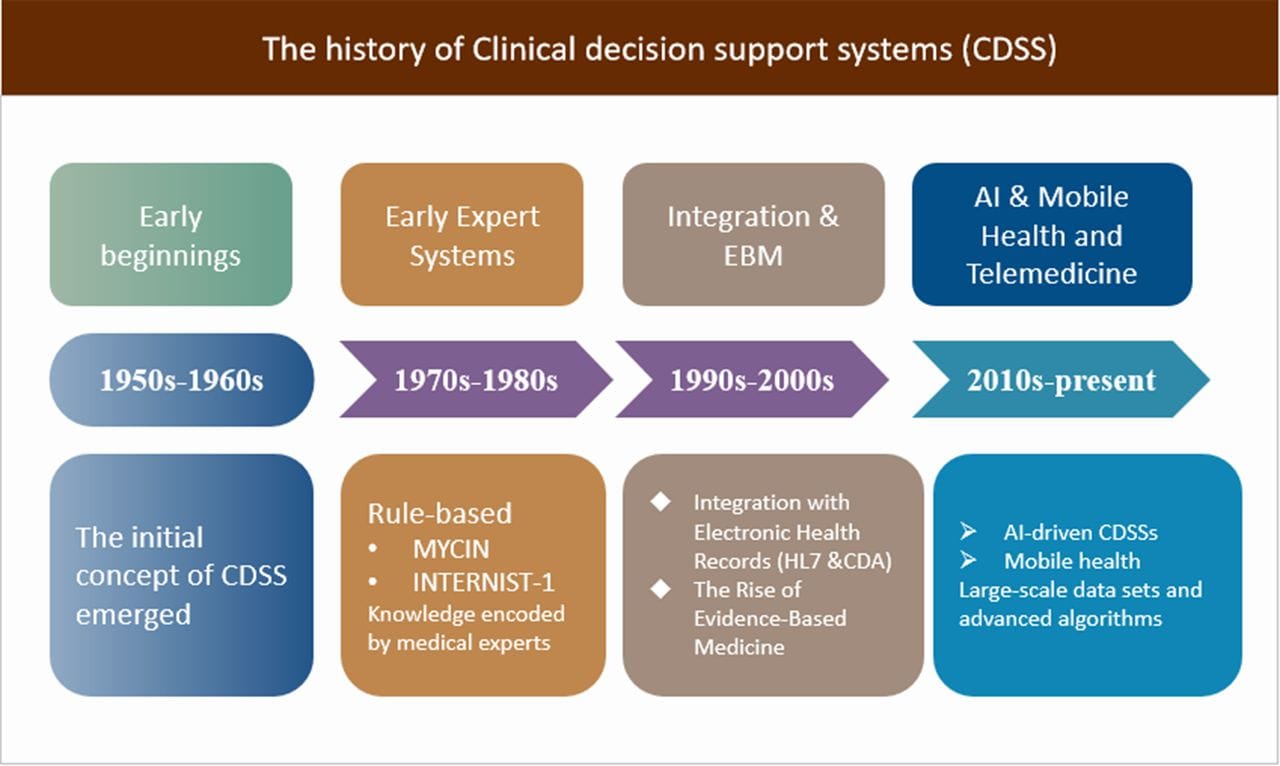
In recent years, the increasing intelligence of artificial intelligence (AI) has led to a novel AI CDS systems. AI technologies, including the likes of natural language processing (NLP), machine learning, and deep learning, have together revolutionized what that CDS can do.
NLP helps CDS to recognize correlations, discern patterns, and come up with insights from incredibly complex datasets. The algorithm is crafted to learn from new data inputs, tweak its predictive capabilities, and adapt as necessary per modern clinical scenario.
On the other hand, NLP - another subset of artificial intelligence helps computers to understand and interpret human language. This is of notable help in the extraction and analysis of valuable information, mainly from unstructured data and electronic health records (EHRs). It can also understand and analyze medical notes as well as medical literature.
Types of clinical decision support systems in healthcare
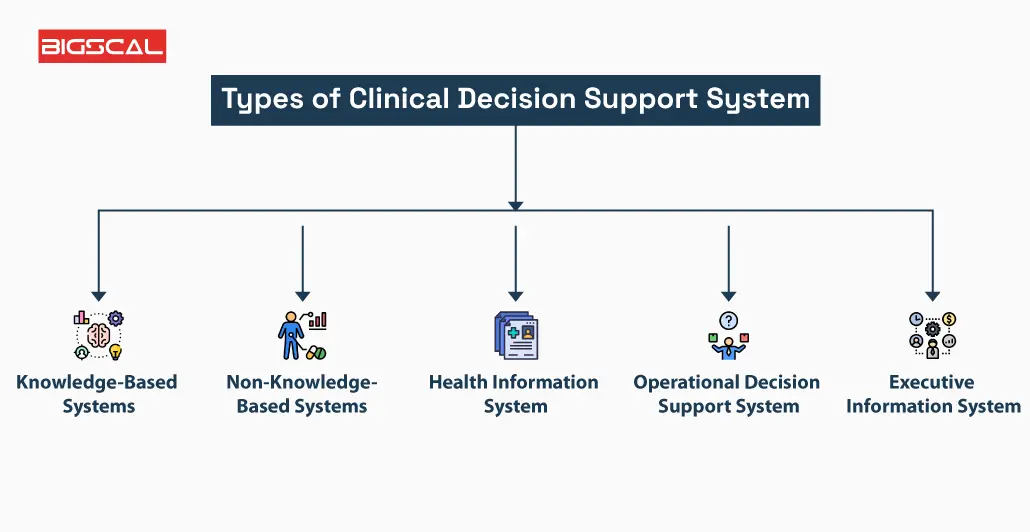
CDS has come a long way since the 1970s when Stanford introduced its first system called MYCIN. Back then, the systems were fairly basic and were designed to help doctors by comparing a patient’s information to a pre-programmed knowledge base. The intent was the same as today, although it was a much cruder version of what we now have. These days, CDS tools are significantly smarter, faster, and more capable of processing all kinds of complex data.
The early systems could be classified as either knowledge-based or non-knowledge-based. Knowledge-based CDS used a set of If-Then rules. For example, if a patient’s blood pressure was high, the system would recommend a certain type of medication. While this sounds great in theory, the if-then rules often lead to documentation burden and cognitive cluttering- slowing down clinical work flows rather than augmenting.
Non-knowledge-based CDS, on the other hand, relies on artificial intelligence and machine learning instead of fixed rules. These systems access large volumes of historical patient data to find patterns and make predictions. Rather than being limited to predefined rules, AI-driven systems learn from real-world data and offer suggestions based on their own analysis.
While both types of CDS are important, AI-powered systems are opening up new possibilities that actually fit into the clinician's workflow. They have evolved significantly over time and are now capable of detecting patterns that even experienced doctors might miss, making them a valuable tool in 2025 and beyond.
Role of AI technology in clinical decision support systems
AI applications in clinical decision support systems
AI has brought about a major revolution in healthcare, especially in CDS. These smart tools/systems make use of artificial intelligence to help doctors and healthcare teams. They help in making better, faster, and more accurate clinical decisions.
Here are the four key areas where AI is making a big impact in CDS.
Diagnostic support
Artificial intelligence helps doctors diagnose diseases more accurately. It analyzes medical images such as MRIs, X-rays, and more using Convolutional Neural Networks to detect issues within the images, often matching or even surpassing human assessments. AI can also scan written clinical notes and use natural language processing to identify important health details that might otherwise go unnoticed, leading to more accurate diagnoses.
Personalized and proactive healthcare
AI in clinical decision support systems helps clinicians create personalized treatment plans based on a patient’s unique health data. It considers medical history, past treatments, and the current story, all of which can influence care decisions. Rather than relying on a one-size-fits-all approach, AI helps determine the most effective treatment for each individual. These tools are also designed to learn over time and continually improve.
Risk prevention and early intervention
AI-powered CDS tools in healthcare are highly effective at identifying high-risk patients before symptoms become obvious. They analyze electronic health records and real-time data to predict conditions such as heart disease or complications from diabetes. This enables clinicians to take early action and prevent serious health issues.
Clinical documentation
AI has significantly reduced the burden of paperwork in healthcare. Advanced systems use voice recognition software to capture what doctors say during patient visits and convert it into accurate documentation. This saves time and makes the process smoother for both clinicians and patients.
CDSS: Impact on patient outcomes
More accurate diagnosis
For conditions like cancer or stroke, timing is everything. This is where AI tools can be of immense value! They help doctors spot problems early, improving chances of successful treatment.
Safer prescriptions
AI can flag dangerous drug interactions before a prescription is even written. It checks patient history, allergies, and even lab results to make sure the meds are safe and properly dosed.
Better use of medical research
CDS tools in healthcare pulls data/ research from multiple studies, giving doctors evidence-based guidance - all in real-time. This thus leads to more standardized, proven treatments and better long-term outcomes for patients.
Spotting health risks early
Access to patient data allows AI tools/systems to predict future health risks - including the likes of heart attack or diabetes complications. Accordingly, it suggests steps such as a change in meds, lifestyle tweaks, or preventative care.
CDS: Impact on operational costs
Fewer errors
Unnecessary tests and diagnostic mistakes can prove expensive. This is where AI-tools shine. With the help of these, doctors can make more accurate diagnoses.
Smoother workflows
In recent years, AI has proved its mettle in handling routine, time-consuming tasks, such as scheduling appointments, entering data, or even drafting patient notes. To add to it, AI can also prioritize patients based on urgency.
Smarter planning
Using past data, AI can predict when hospitals will be the busiest. This thus helps in planning, allowing hospitals/ healthcare facilities to bring in more staff or stock up on supplies when needed and avoid overstaffing when things are slow.
CDS: Challenges and the road ahead
Artificial intelligence is reshaping the healthcare sector - especially when it comes to CDS. These tools help doctors make better decisions by analyzing data quickly and accurately. However, it is necessary to stay clear of tools/systems which give results without clearly showing how they reached them. Using such unreliable tools can be a problem. Why? Because doctors need to know the why and how a recommendation is made before acting on it. This is why DocAssistant's unique citation based approach is not only novel but necessary.
Another challenge that CDS tools face is fitting into the existing healthcare workflows. Doctors or healthcare professionals may be skeptical at first - that these systems might take away their decision-making power or disrupt their routines - but that couldn’t be further from the truth.
To change their perspective, modern AI-powered tools need to be user-friendly and built to support clinicians. Proper onboarding and thoughtful design will help clinicians to adopt and implement these game changing tools.
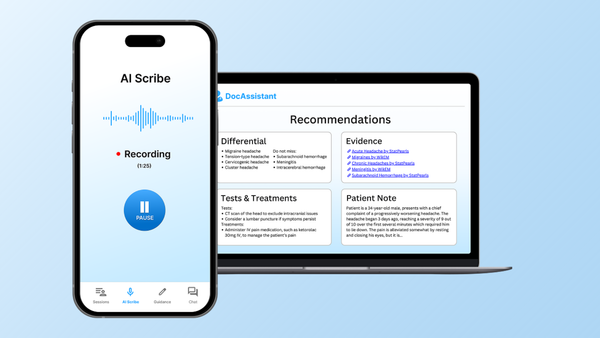
DocAssistant: Usable and Trustable
AI is transforming healthcare, but for these tools to truly deliver impact, they must be designed around the needs of the people using them- clinicians, nurses, and other frontline professionals. That’s why user-centric design is essential. Effective tools must be intuitive, trustworthy, and seamlessly integrated into everyday clinical workflows. DocAssistant is built with this philosophy at its core. It delivers evidence-based recommendations supported by clickable source links, allowing clinicians to explore the rationale behind each suggestion and dive deeper into associated diagnoses, workups, and treatment pathways. Combined with a powerful AI scribe that dramatically reduces documentation time and automatically provides deep patient specific context for the CDS tool, DocAssistant stands out as a uniquely reliable and efficient clinical decision support (CDS) platform.
Built by clinicians, for clinicians. Try out DocAssistant today.
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an emergency medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about leveraging AI to streamline administrative tasks and enhance clinical decision making