Choosing Between AI and Human Scribes for Better Clinical Workflow

In today’s healthcare environment, physicians are responsible for much more than diagnosing and treating patients. A substantial portion of their time is spent entering information into Electronic Health Records. Research shows that many doctors now spend more time on documentation than with patients, contributing to dissatisfaction and burnout.
To help ease this burden, many healthcare practices are turning to medical scribes, whether human or powered by artificial intelligence. As both options become more widely available, decision-makers must weigh the cost, efficiency, and reliability of each.
This article outlines the key differences between AI and human scribes and offers guidance on selecting the right fit for your practice.
The Growth of Medical Scribes in Healthcare
While medical scribes have existed for decades, their role has significantly expanded over the past 20 years. In the early 2000s, as policies like the HITECH Act made Electronic Health Records mandatory, many physicians began to feel overwhelmed by administrative tasks. Human scribes became more common, assisting by documenting patient interactions in real time. By 2014, there were more than 20,000 medical scribes working in the United States, with that number continuing to rise.
In the late 2010s, advances in natural language processing and machine learning gave rise to AI scribes. Initially focused on basic transcription, these tools have since evolved to capture speech in real time, generate clinical summaries automatically, and integrate directly with EHR systems. As a result, AI scribes have emerged as a scalable alternative to human scribes for many healthcare practices.
The Growing Burden of Clinical Documentation
Electronic Health Records were introduced to improve the quality and accessibility of patient information, but they have also added to the administrative workload for clinicians. Recent studies show that physicians spend an average of 16 minutes per patient visit on documentation alone. This figure does not include the additional hours many spend completing notes at home, often referred to as “pajama time.”
Research further indicates that for every hour spent on patient care, nearly two hours are devoted to EHR-related tasks and desk work. This imbalance can reduce meaningful patient interaction and contribute to clinician fatigue and burnout.
To address these challenges, both human and AI-powered medical scribes are being adopted across a growing number of specialties. These tools are designed to relieve documentation pressure and help providers reclaim time for direct patient care.
Understanding Human Medical Scribes
A human medical scribe is trained to follow a physician during patient visits, either in person or remotely, and document key details in real time. Under the physician’s direction, scribes enter patient histories, examination findings, diagnostic tests, and treatment plans into the Electronic Health Record.
Benefits of Human Scribes
Human scribes are skilled at interpreting complex medical conversations. They can adapt to a physician’s specific language, abbreviations, and contextual cues, producing accurate and personalized documentation. As familiarity grows, the collaboration between doctor and scribe often leads to faster and more precise charting.
Their versatility is another advantage. Whether working in cardiology, mental health, or another specialty, experienced scribes can tailor their approach to fit the clinical setting. They are also better equipped to handle unexpected changes during a visit compared to many digital alternatives.
In addition to improving workflow, human scribes can enhance the patient experience. By managing documentation, they allow physicians to focus more fully on the patient rather than the computer screen, supporting better communication and more engaged care.
Glaring Limitations of Human Scribes
While human scribes offer valuable support, they also come with notable challenges. Cost is a primary concern. Recent estimates show that hiring a scribe can range from $2,500 to $4,500 per month, depending on whether the role is full-time or part-time. For smaller practices, this represents a substantial ongoing expense.
Turnover is another common issue. Many scribes are pre-medical students seeking clinical experience before applying to medical school, which means they often stay for only one to two years. High turnover creates a need for continuous training and onboarding, which can disrupt workflow and place added strain on clinical staff.
Scaling human scribe programs across multiple providers or locations is also complex. Expanding coverage requires recruiting, training, and managing additional staff, which may be difficult for rapidly growing or multi-site practices.
What Is an AI Medical Scribe
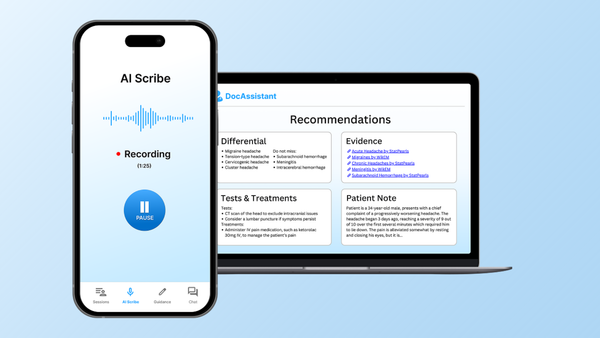
An AI medical scribe is a digital tool that uses natural language processing and machine learning to generate clinical documentation. These systems capture doctor-patient conversations through a microphone, telehealth platform, or wearable device and then produce structured notes ready for entry into the Electronic Health Record.
Advantages of AI Scribes
AI scribes offer consistent availability, operating around the clock without breaks. This makes them especially valuable for practices with extended hours, high patient volumes, or providers working across different time zones.
They are also highly scalable. A single software license can support multiple physicians without the need for hiring, training, or managing additional staff. Once implemented, AI scribes can be quickly deployed across teams or locations, making them one of the most flexible documentation solutions available.
In terms of cost, AI scribes are typically more affordable than human scribes. Most are offered through subscription-based models, which often cost less than employing full-time personnel.
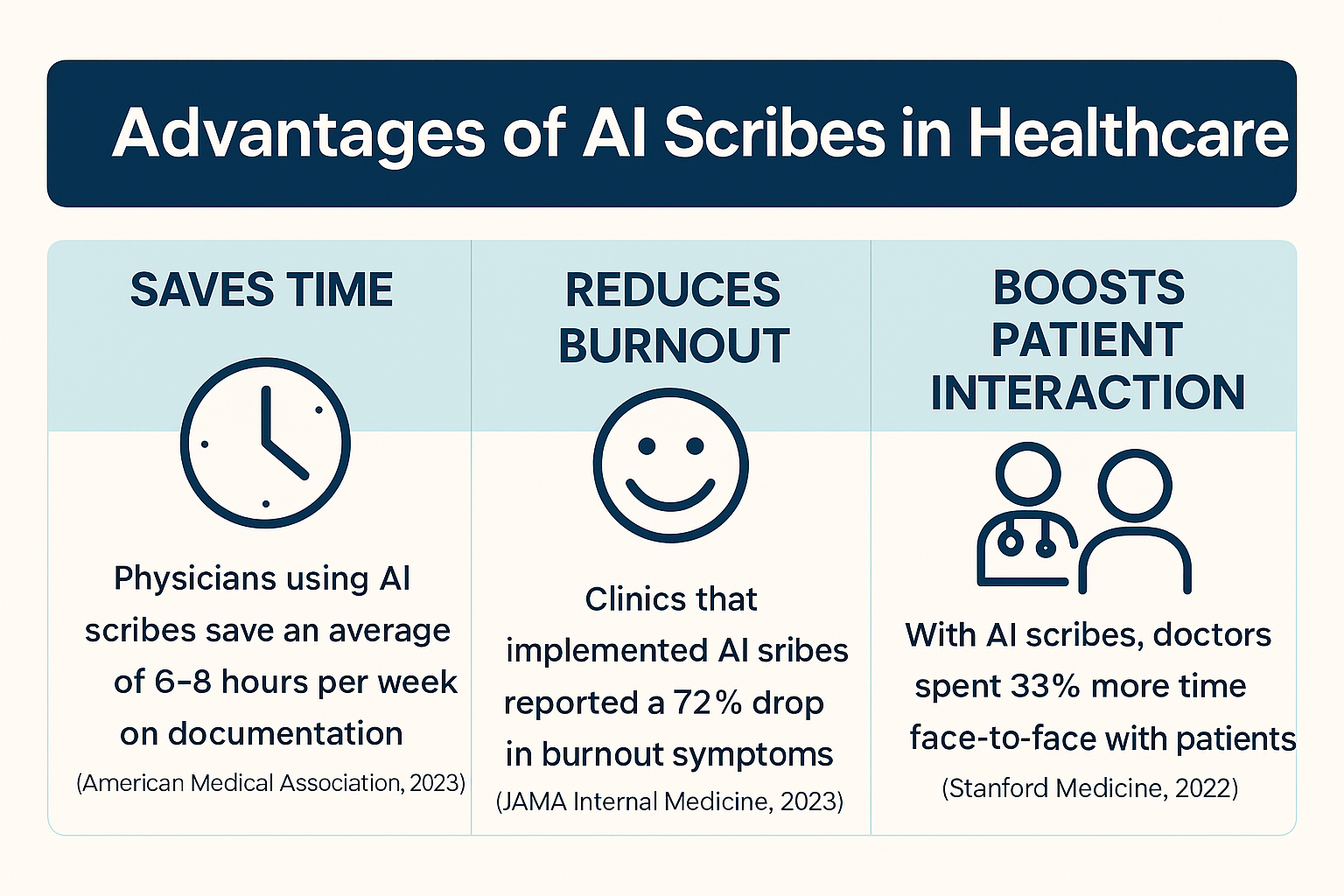
AI scribes also accelerate the documentation process. In many cases, notes are generated immediately after a visit, reducing the need for after-hours charting. This can support better work-life balance for providers and help alleviate long-term burnout.
Limitations of AI Scribes
While AI scribes offer valuable support, they are not perfect just yet. Speech recognition can be inconsistent in noisy environments, with overlapping conversations, or when dealing with diverse accents. These issues may result in transcription errors that require manual correction.
Privacy and security remain critical concerns. AI scribes must safeguard patient information through robust encryption, secure data handling, and strict adherence to HIPAA regulations.
Additionally, not all AI scribes integrate seamlessly with Electronic Health Records. Some require additional software or workflow changes, which can introduce complexity and increase implementation costs.
Scribes and Physician Burnout
Physician burnout is a growing concern that affects both provider well-being and the quality of patient care. According to a recent study by the American Medical Association, more than 60 percent of physicians reported feeling burned out in 2022, with much of the stress linked to the demands of electronic health records.
Research indicates that medical scribes, whether human or AI, can help reduce the documentation burden and improve physician job satisfaction. By offloading administrative tasks, scribes allow providers to focus more on patient care and spend less time on after-hours paperwork.
Although AI scribes are still a relatively new solution, early results are promising. Initial programs suggest that when used consistently, AI scribes can significantly reduce documentation-related stress and contribute to a more sustainable work environment for clinicians.
Legal and Compliance Considerations
Whether working with human or AI scribes, compliance with HIPAA and relevant privacy regulations is essential.
- Voice Recording and Consent
Some states require all parties to consent before recording conversations, including in clinical settings. Practices using AI scribes with audio capture should verify state-specific laws and obtain proper consent.
- Data Storage and Access Control
AI scribe vendors must use strong data encryption, enforce strict access controls, and maintain detailed logs of data access. For human scribes, practices should have signed Business Associate Agreements, ensure HIPAA training, and implement secure login protocols.
- Liability and Documentation Accuracy
Physicians remain ultimately responsible for the accuracy of clinical documentation, regardless of who or what generated it. Regularly reviewing all notes helps minimize legal exposure and ensures clinical accuracy.
How to Evaluate Scribe Solutions
Before selecting a scribe solution, it is important to assess how well it aligns with your clinical, technical, and operational needs. The following checklist can help guide the evaluation process:
- Turnaround Time
Determine whether notes are available in real time or how quickly finalized documentation is delivered after the visit.
- Specialty Adaptability
Assess whether the solution performs well in your specific clinical environment and can manage both structured formats and conversational documentation.
- Accuracy and Editing Requirements
Review the typical error rate and evaluate how much editing is needed before notes can be finalized and signed off.
- Compliance and Security
Ensure the solution meets HIPAA requirements, including secure data handling, encryption protocols, and access logs.
- Trial Access and Support
Look for a trial period to test the system in your workflow, and confirm that technical support or onboarding assistance is available.
Taking the time to evaluate these factors can help your practice avoid costly missteps and ensure the selected solution aligns with clinical goals and documentation standards.
Operational Considerations and Hidden Costs
Both human and AI scribes offer valuable support, but each comes with potential hidden costs that practices should consider when planning their investment.
For Human Scribes
- Time and resources are required for recruitment, training, and day-to-day management
- On-site scribes may need dedicated workspace, computers, or other tools
- High turnover can result in lost institutional knowledge and repeated training expenses
For AI Scribes
- Initial setup may require support from IT professionals, especially for integration with existing systems
- Ongoing subscription fees may include added costs for technical support or advanced features
- Additional equipment such as microphones or ambient sensors may be necessary for optimal performance
Understanding these operational factors can help practices budget more accurately and avoid unexpected challenges during implementation.
Patient Perception
Patient comfort and trust are essential when introducing scribe solutions. Research shows that most patients are comfortable with a human scribe present during their visit, especially when they understand the scribe’s role and know their privacy will be respected. AI scribes are generally less noticeable, but transparency remains important. Patients should be informed when AI tools are in use and how their data will be handled. In some cases, consent may be required for audio recording, depending on local laws and practice policies.
The Future of Scribing: Hybrid Models and Advancing Technology
Many healthcare organizations are moving toward hybrid models that combine the strengths of both human and AI scribes. In these models, AI tools manage routine note-taking while human scribes provide oversight and handle more complex cases. This blended approach balances efficiency with accuracy and flexibility.
AI technology continues to evolve, with improvements in voice recognition, coding assistance, and adaptability to individual physician workflows. As these systems become more refined, hybrid models offer a promising path forward by merging the reliability of human insight with the scalability of automation.
Conclusion
Choosing between an AI scribe and a human scribe depends on your practice’s needs, including patient volume, clinical complexity, budget, and comfort with technology. Human scribes excel in complex or unpredictable situations, offering flexibility and nuanced understanding. AI scribes, on the other hand, are more cost-effective, and scalable.
As hybrid models gain traction and AI technology continues to evolve, combining both approaches may offer the most balanced and effective solution. Together, they represent a strong set of options that can reduce administrative burden and help physicians refocus on patient care.
For practices looking to adopt a high-quality AI scribe, DocAssistant offers a comprehensive solution. It goes beyond basic transcription by also offering a point of care revenue cycle management (RCM) tool and clinical decision support (CDS) arm as well. Try it out today!
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline medical documentation and enhance clinical decision making.