AI in Emergency Medicine: Boosting Reimbursement and Elevating Care
Artificial intelligence has entered many industries, including healthcare. In medicine, AI helps improve accuracy, enhance patient safety, reduce workload, and support faster clinical decisions. It is also becoming increasingly important in managing administrative tasks.
In the fast-paced environment of the emergency department, these capabilities are especially valuable for improving patient outcomes. Beyond clinical support, AI can also help optimize reimbursement and reduce clinician burnout.
This article explores the key benefits and applications of AI in emergency medicine.
AI Optimizing Reimbursement
Optimizing reimbursement is essential for maintaining the sustainability of healthcare services, and AI can play a key role in supporting that goal.
AI tools can:
- Suggest codes that reflect the full complexity of care provided
- Recognize billable procedures in real-time such as imaging, labs, and wound care
- Identify incorrect or incomplete codes before submission
Reducing medical coding errors can lead to increased reimbursement. A report from the American Medical Association estimates that coding errors in the U.S. healthcare system account for approximately $36 billion in lost revenue each year.
AI clinical tools can also enhance documentation quality. More accurate and complete documentation often results in higher diagnosis-related group (DRG) assignment, which can directly impact reimbursement.
Improved documentation may include:
- Offering real-time prompts to capture missing information
- Flagging charting discrepancies that could result in undercoding
- Alerting clinicians to missed billing opportunities
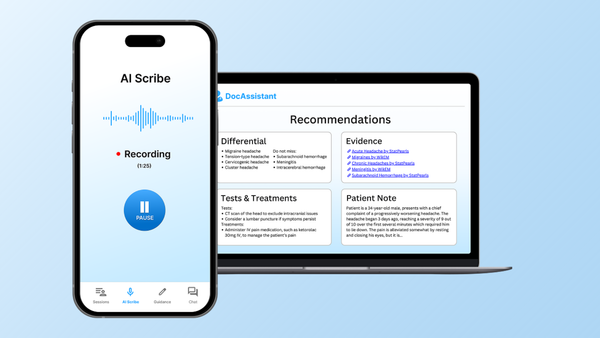
A case study conducted with Elite Hospital Partners found that emergency medicine physicians using DocAssistant’s HIPAA-compliant AI Co-Pilot reduced their charting time by 85% and improving revenue by 8%.
Unlike generic transcription tools, AI scribes built specifically for emergency medicine are designed to meet the fast-paced demands of the ER. These systems capture key clinical details in real time, helping ensure nothing is missed.
How AI Can Transform Care
In addition to improving reimbursement, one of the most exciting aspects of AI is its potential to transform clinical care. While AI will never replace clinical judgment, it can serve as a valuable tool to support decision-making and enhance patient outcomes.
Triage and Risk Assessment
In emergency medicine, AI can help streamline triage by reducing the time from arrival to initial assessment. By analyzing a patient’s medical history, symptoms, and vital signs, AI tools can assess severity and predict the risk of clinical deterioration in real time.
One of AI’s unique strengths is its ability to interpret patient-reported symptoms during registration and link them to relevant clinical pathways. For example, if a patient says, “My chest is tight and I can’t breathe,” the system may flag potential high-risk diagnoses such as sepsis, pulmonary embolism, or stroke—prompting faster evaluation and treatment.
AI systems can also continuously monitor vital signs and detect early warning signs while a patient is waiting. If a condition worsens, the system automatically alerts clinical staff.
In addition, AI may assist in assigning Emergency Severity Index (ESI) levels more objectively and consistently than human providers. This can improve triage accuracy and patient prioritization, supporting more efficient patient flow.
Diagnostic Support
AI can play a valuable role in diagnostic support, particularly during periods of high patient volume. These tools can quickly surface essential information such as drug interactions, lab trends, and patterns in clinical data. In doing so, AI may suggest potential diagnoses or prompt clinicians to consider alternative explanations, helping to ensure that nothing is overlooked.
In high-pressure environments like the emergency department, clinicians may sometimes fixate on an initial diagnosis. AI can help mitigate this risk by identifying inconsistencies in the data that may point to other possibilities. By providing objective, data-driven prompts, AI serves as a second set of eyes -unaffected by fatigue or cognitive bias - supporting clinical judgment rather than replacing it.
Improving Patient Flow
High patient volumes and long wait times present ongoing challenges for both clinicians and patients. AI tools can support more efficient patient flow, which helps improve the quality of care and overall patient experience.
For instance, AI-powered systems can streamline the registration and triage process, making the intake experience faster and more effective. These systems can also analyze patterns in patient movement to predict busy periods, suggest appropriate staffing adjustments, and reduce care delivery bottlenecks. This makes emergency departments more organized and eases the daily pressure on clinical teams.
In addition, automating routine administrative work such as intake documentation and discharge instructions helps reduce the workload on staff and supports a more coordinated, less chaotic environment.
AI as a Tool in Reducing Burnout
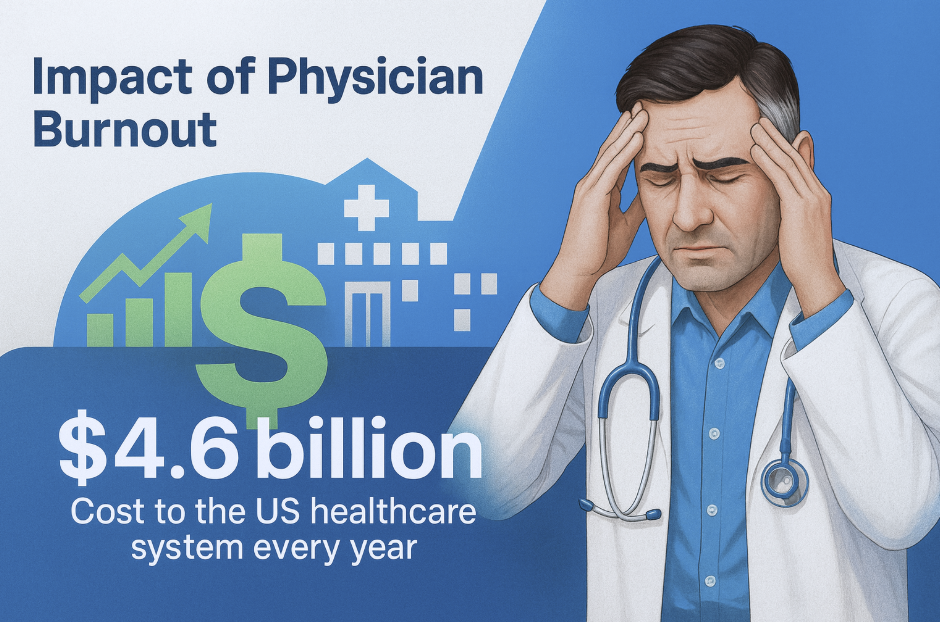
One of the most promising benefits of AI in the emergency room is its ability to reduce some of the key pressures that contribute to clinical burnout.
According to the Mayo Clinic, burnout has both personal and financial consequences. In the United States, physician burnout is estimated to cost the healthcare system approximately $4.6 billion annually.
Emergency physicians often face burnout due to high patient volumes, long shifts, and a heavy documentation burden. In fact, they experience one of the highest documentation workloads among healthcare providers. AI can help alleviate this by reducing the time spent charting and simplifying the documentation process. Many tools generate notes automatically, including sections such as history of present illness, review of systems, and physical exam findings.
Compared to generic dictation tools, AI scribes designed specifically for emergency medicine often provide more accurate results, reducing errors and improving efficiency. This allows physicians to complete documentation more quickly and devote more attention to patient care, collaboration with peers, and restorative downtime.
Clinical decision support powered by AI can also help speed up decision-making and reduce cognitive fatigue. By helping to confirm diagnoses or highlight uncertainties, AI contributes to a more confident and less stressful clinical environment.
Even saving one or two hours per shift can add up to hundreds of hours annually. That time can be redirected toward family, personal interests, or rest - key elements in achieving a healthier work-life balance. In a demanding field like emergency medicine, preserving long-term wellbeing is essential, and AI has the potential to support that goal.
Challenges and Limitations of AI in Emergency Medicine
As discussed, AI in emergency medicine offers powerful opportunities to improve workflow, enhance reimbursement, and elevate patient care. However, several limitations and barriers may impact its broader adoption.
One critical factor is how AI aligns with evolving reimbursement pathways. As healthcare payment models continue to change, AI tools must keep pace with documentation and billing requirements. A lack of standardization and inconsistent payer acceptance can create challenges. In some cases, payers may deny claims if the use of AI is not clearly documented or validated. Ensuring transparency in how AI supports documentation and care will be essential for building trust and avoiding reimbursement issues.
Implementing AI in the emergency department may also involve upfront costs. These may include:
- The purchasing or licensing AI software
- Configuring the system to fit existing clinical workflows
- Training staff to use it effectively
It is equally important to acknowledge that AI is not error-proof. Mistakes can occur, and without proper oversight, overreliance on AI could gradually erode clinical judgment. Ultimately, clinicians remain responsible for patient care, and their engagement in reviewing and validating AI-generated outputs is essential to ensuring accuracy and safety.
Conclusion
AI is rapidly becoming a powerful asset in emergency medicine, supporting both financial and clinical outcomes. From optimizing reimbursement through improved documentation to streamlining workflows and enhancing diagnostic support, AI has the potential to elevate care delivery in high-pressure environments.
Beyond operational efficiency, AI can ease documentation burdens and help reduce physician burnout by allowing clinicians to focus more time and energy on what matters most - providing attentive, compassionate care. Still, it is not a replacement for clinical judgment or the human connection at the core of emergency medicine.
As the technology evolves, AI is expected to play an increasingly important role in improving patient care, optimizing emergency department operations, and shaping the future of emergency medicine.
About the Author
Nathan Murray, M.D. Emergency Medicine - Founder of DocAssistant
Dr. Nathan Murray is an Emergency Medicine trained physician and the founder of DocAssistant. With years of frontline clinical experience, Dr. Murray is passionate about using AI to streamline medical documentation and enhance clinical decision making.